Glenoid Labral Tears
- Home
- Conditions
- Shoulder pain
- Glenoid Labral Tears
Glenoid labral tears are a common cause of shoulder pain in the society and is commonly found in association with other shoulder pathologies like rotator cuff tears, impingement and glemohumeral arthritis. Hence many a times glenoid labral tears can go unnoticed. While certain labral tears obviate an Arthroscopic repair, there is a large number of cases which respond favourably to regenerative injection techniques like Comprehensive Platelet Rich Plasma with Prolotherapy.
Glenoid Labrum: Anatomy & Function
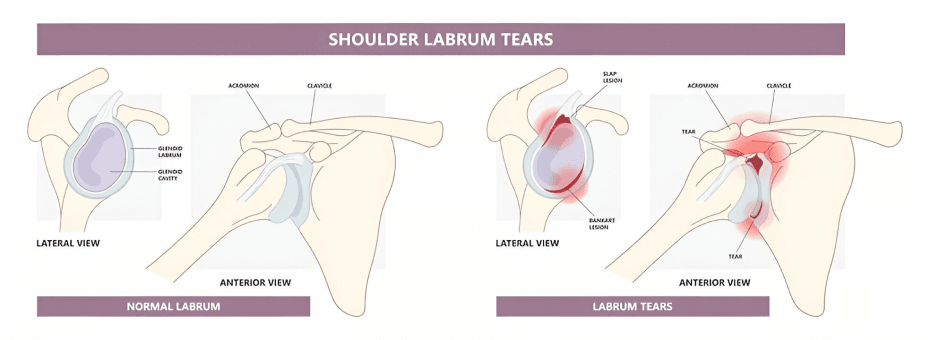
A rim of fibrocartilaginous tissue running along the rim of the glenoid fossa represents the glenoid labrum. The labrum continues into the articular cartilage inferiorly but superiorly is subject to aberrant morphologies causing the labral attachment to the cartilage to be either firm, loose or absent. It also serves as an attachment site for the biceps tendon and the glenohumeral ligament.
The labrum serves the function of adding stability to the glenohumeral joint. The joint is specifically shaped with the humeral head articulating with concave glenoid fossa. This joint optimises range of motion over stability as the humeral head is about 4 times the size of the glenoid cavity. The labrum enhances the glenoid coverage resulting in augmentation of the contact between the articulating surfaces. This results in added concavity of the fossa increasing the inherent strength of the joint. Stabilisation is further enhanced by the labral anchorage of the biceps, triceps and capsuloligaments. The labrum also prevents shoulder dislocation by acting as a seal and maintaining negative intra- articular pressure. Further, the glenoid labrum is more vascular on the peripheries as opposed to the centre which poses challenges for certain labral tears to heal.
Lesions of the Glenoid Labrum
- Forceful abduction,extension and external rotation can cause avulsion of the anterior labrum.
- Forceful abduction,extension and external rotation can cause avulsion of the anterior labrum.
- Axial loading of an adducted and internally rotated arm can bring about a posterior avulsion of the labrum.
- Chronic repetitive overload as happens with athletes playing overhead sports, can lead to tears. These might be accompanied by degeneration in the joint as well as degeneration of the labrum itself
Types of Lesions
- Morphologically labral tears can be classified as Flap tears, Incomplete split tears, bucket handle tears and Superior Labral Anterior and Posterior( SLAP) tears.
- Bankart described a lesion in the antero-inferior part of the joint causing detachment of the capsule with the glenoid labrum, commonly seen with chronic repetitive overhead use.
- SLAP tears have been a topic of importance as they are commonly observed in high performance athletes.The most common SLAP lesions notably are the type II, in which the superior labrum and biceps tendon are each detached from the glenoid. The wide spectrum of SLAP lesions poses difficulties in management of patients with labral tear. Type I SLAP tears, for example, constituting approximately 20 percent of SLAP lesions show a high association with rotator cuff lesions, and are considered of low clinical relevance. Surgery for these patients may not be indicated. However, type I SLAP tears are difficult to distinguish from type III and type IV preoperatively. Consequently, inaccurate diagnosis can result in unnecessary arthroscopy. While labral tears can occur in isolation, the majority of tears are found in the context of additional glenohumeral pathology like impingement, instability and rotator cuff lesions.
Diagnosis
Careful history and clinical examination can give telling clues to our diagnosis. Patient history may indicate relevant acute events or sources of chronic stress. Patient often complain of popping, clicking or catching hinting towards the diagnosis of labral tear.
The physical tests used for diagnosis are the crank test, the active compression (O’Brien) test, the anterior slide test, the anterior apprehension test, Speed’s test, Jobe’s relocation test, and testing for tenderness in the bicipital groove. Often these tests are used together have shown higher sensitivity than doing the tests alone.

Treatment
Conservative treatment in the form of rest, analgesics and physical therapy focusing on capsular stretching and muscle strengthening is often the initial approach.
Arthroscopic repair has been used especially in the frequent SLAP II Type lesions. The repair involves refixation to the glenoid using a suture anchor technique. Bankart’s lesions posing with instability and other degenerative lesions are also often subjected to Bankart’s repair .
At Alleviate
We follow an approach of Image guided Comprehensive Platelet Rich Plasma with Prolotherapy for patients who are not candidates for surgery and those who have failed initial conservative attempts. These indeed form a huge subset of patients with labral pathology. Treatment is concentrated on the posterior joint capsule, the supraspinatus, infraspinatus and teres minor tendons, and the glenohumeral, coracohumeral and acromioclavicular ligaments.This is followed by glenohumeral joint injection. The treatment is carried out under Ultrasound and at times Fluoroscopic guidance as well.
We couple this with a dedicated physical therapy and shoulder rehabilitation programme as well.
FAQs - Glenoid Labral Tears
A Glenoid labral tear, also known as a glenoid labrum tear is a tear in the labrum of the shoulder joint, which is a ring of cartilage that helps to stabilize and deepen the joint.
Shoulder pain is a prevalent condition among the population, often attributed to Glenoid labral tears. It is frequently associated with other shoulder pathologies, such as rotator cuff tears, impingement and glenohumeral arthritis.
Symptoms of a glenoid labral tear can include shoulder pain, instability, limited range of motion, and a clicking or popping sensation.
A common cause of a Glenoid labral tear in the shoulder can be traumatic incidents or repetitive motion.
Glenoid labral tear causes:
- Fall or an accident
- Overuse of muscles and tendons
- Injury to the shoulder joint
- Instability of the shoulder joint
- Wear and tear on the shoulder joint
- Repetitive activities involving lifting or throwing
- Degenerative condition such as arthritis
Lesions of the glenoid labrum are pathologic changes in the cartilage of the glenoid cavity of the shoulder joint. These lesions may be caused by trauma or degenerative changes and can lead to shoulder instability, pain, and reduced range of motion.
A careful history and clinical examination can help to diagnose a labral tear by looking for signs and symptoms related with the condition, such as pain or clicking with specific movements, decreased range of motion, and a feeling of instability or weakness.
Additionally, physical tests can be used to confirm the diagnosis.
Physical tests utilized for diagnosis include
- The Crank Test
- O'Brien's Active Compression Test
- Anterior Slide Test
- Anterior Apprehension Test
- Speed's Test
- Jobe's Relocation Test
- Bicipital Groove Tenderness Test
Types of lesions include as follows:
- Morphologically labral tears – a tear that occurs in a specific labral shape or pattern.
- Bankart lesion – a tear occurs in front of the labrum of the shoulder
- SLAP tears – a tear from the superior labrum from anterior and posterior tears
The best possible treatments for glenoid labral tears depend on the severity of the injury, the patient's age, and the overall health of the patient. Treatments may include rest, physical therapy, and anti-inflammatory medications focussing on reducing pain and muscle strengthening.
Yes. If the conservative forms of treatment fail, a minimally invasive technique is required. Arthroscopic repair involves fixing a glenoid tear using a suture and a device to make a small incision.
Treatment for Bankart's lesions typically involves surgical stabilization of the shoulder joint, such as a Bankart repair or Latarjet procedure.
At Alleviate, we use Imaged Guided Comprehensive Platelet Rich Plasma with Prolotherapy to treat patients who are not suitable for surgery and have not found successful results from conservative treatments.
The therapeutic at Alleviate focus on the posterior joint capsule, the supraspinatus, infraspinatus, and teres minor tendons, as well as the glenohumeral, coracohumeral, and acromioclavicular ligaments.
A glenohumeral joint injection is then administered, which is carried out using Ultrasound and sometimes Fluoroscopic guidance.
Video Spotlight
Blog
Surgery-Free Solutions
Expert Tips for Pain Management
Testimonials
Words From Our Patients
In this clinic, Chaitra Physiotherapist did a great job for me, as i’ve been suffering from shoulder pain. She did dry needling and stretching exercises, so much relieved from pain. Thank you so much
I have taken treatment for shoulder pain here by Dr Wiquar Ahmed and I get relief, now I am so happy. My wife has been undergoing P R P therapy treatment for knee pain, she is gradually recovering from the pain. we hope the treatments will give better results. Particularly for knee pain, it is better to take PRP rather than knee replacement so that we may postpone the knee replacement.
There are Great doctors here. I suffered from shoulder pain for a year. After coming to alleviate pain, the pain is completely gone. I took two PRP sessions and physiotherapy. The physiotherapist are also amazing.
I had pain on the right side of my neck and shoulder. Dr Akhila, Dr Hemashree and Dr Chaithra have given me the right physiotherapy treatment for 7 days , they also taught me exercises to fix my posture and stop injuries from arising in the future. Now I feel much better and my body feels free.