Introduction
Knee pain is a prevalent issue that can significantly impact the quality of life for many individuals. Knee Osteoarthritis, Ligament injuries and Chondromalacia Patella are the commonest causes of adult knee pain.Traditional treatments often involve medications, physical therapy, or even surgery. However,
Platelet-Rich Plasma (PRP) therapy has emerged as a promising alternative for knee pain management, providing patients with a non-surgical, minimally invasive option.

PREPARATION OF PLATELET RICH PLASMA
The process of blood collection, centrifugation, and isolation of platelet-rich plasma (PRP) involves several steps to obtain a concentrated solution rich in platelets, growth factors, and other bioactive proteins. Here’s a detailed overview of each stage:
Blood Collection
The process begins with the collection of a small volume of whole blood from the patient. Typically, the blood is drawn from a vein in the arm using a sterile needle and collected into specialized tubes or syringes containing anticoagulants to prevent clotting.
Centrifugation
Once the blood is collected, it undergoes centrifugation, a process that separates its components based on their densities. During centrifugation, the blood sample is placed in a centrifuge machine, which spins rapidly, causing the heavier components to settle at the bottom while the lighter components rise to the top.
Buffy Coat Extraction
 PRP PREPARATION AT ALLEVIATE PAIN CLINIC
PRP PREPARATION AT ALLEVIATE PAIN CLINIC After centrifugation, the blood separates into three distinct layers:
- Red Blood Cells (RBCs): These are the heaviest components and settle at the bottom of the tube.
- Plasma: The liquid portion of the blood containing water, electrolytes, and proteins. It occupies the middle layer.
- Buffy Coat: This thin, whitish layer lies between the red blood cells and the plasma. It contains platelets, white blood cells, and some residual red blood cells.
Separation of Platelets
The next step involves carefully extracting the buffy coat layer, which contains a higher concentration of platelets compared to the other blood components. The buffy coat is separated from the rest of the blood using specialized tools or pipettes.
Platelet-Rich Plasma (PRP)
Once the buffy coat is isolated, it undergoes further processing to obtain platelet-rich plasma. This involves resuspending the buffy coat in a small volume of plasma, which helps concentrate the platelets while removing excess red blood cells and white blood cells.
Ideal Color and Consistency of PRP
The ideal color and consistency of PRP can vary depending on factors such as the patient’s hematocrit levels, platelet count, and the specific centrifugation protocol used. However, in general, PRP should exhibit the following characteristics:
- Color: PRP typically has a straw-colored or slightly amber appearance. The presence of a reddish tint may indicate residual red blood cells, while a milky appearance suggests a high concentration of white blood cells.
- Consistency: PRP should have a relatively thin consistency similar to that of whole blood. It should be free-flowing and easily injectable, allowing for precise administration into the target site.
- Platelet Concentration: The concentration of platelets in PRP can vary depending on the specific protocol used. However, ideal PRP formulations often contain platelet concentrations several times higher than that of whole blood, typically ranging from 3 to 5 times baseline levels.
- Absence of Clots: PRP should be free of clots or fibrin strands, which can impede the injection process and affect its efficacy.

HOW PRP HELPS WITH KNEE PAIN? -MECHANISM OF ACTION
Inflammation Modulation
Chronic inflammation plays a key role in the progression of knee OA, contributing to pain, cartilage degradation, and joint dysfunction. PRP contains numerous anti-inflammatory cytokines and growth factors that help modulate the inflammatory response within the joint microenvironment.
- TGF-β (Transforming Growth Factor Beta): TGF-β is a potent anti-inflammatory cytokine found in PRP that helps regulate immune cell activity and suppress pro-inflammatory pathways.
- Interleukin-1 Receptor Antagonist (IL-1Ra): IL-1Ra is another important component of PRP that competes with pro-inflammatory cytokines like IL-1 for binding sites, thereby mitigating their inflammatory effects.
Growth Factor Stimulation
PRP is rich in various growth factors that play crucial roles in tissue repair, regeneration, and remodeling. These growth factors act synergistically to promote healing and enhance the intrinsic repair mechanisms within the knee joint.
- Platelet-Derived Growth Factor (PDGF): PDGF stimulates cell proliferation, angiogenesis, and extracellular matrix synthesis, contributing to tissue regeneration and repair.
- Insulin-Like Growth Factor-1 (IGF-1): IGF-1 promotes chondrocyte proliferation and matrix synthesis, thereby supporting cartilage repair and maintenance.
Cartilage Repair
One of the primary goals of PRP therapy in knee OA is to promote cartilage repair and regeneration, thereby slowing down disease progression and improving joint function.
- Stimulation of Chondrocyte Activity: PRP contains bioactive factors that stimulate the metabolic activity of chondrocytes, the primary cells responsible for cartilage maintenance, leading to enhanced matrix production and repair.
- Enhanced Matrix Formation: Growth factors present in PRP promote the synthesis of extracellular matrix components such as collagen and proteoglycans, which are essential for cartilage integrity and resilience.
Improving Overall Joint Health
PRP therapy not only targets specific pathological processes within the knee joint but also contributes to overall joint health and function by promoting tissue healing, reducing pain, and enhancing mobility.
- Angiogenesis and Tissue Remodeling: PRP promotes angiogenesis, the formation of new blood vessels, which facilitates nutrient and oxygen delivery to the injured tissues, supporting healing and remodeling processes.
- Pain Reduction: By modulating inflammation, promoting tissue repair, and stimulating neuroregenerative processes, PRP therapy can help alleviate pain associated with knee OA, improving patients’ quality of life and functional outcomes.
Combination with Prolotherapy
At Alleviate, the combination of PRP with prolotherapy offers a comprehensive approach to knee OA treatment. Prolotherapy involves the injection of a proliferant solution, such as dextrose, to induce controlled inflammation and stimulate tissue repair mechanisms.
- Synergistic Effects: Combining PRP with prolotherapy may enhance the therapeutic efficacy by synergistically promoting tissue regeneration, modulating inflammation, and improving joint stability.
- Long-Term Benefits: The combined approach addresses multiple aspects of knee OA pathophysiology, potentially leading to sustained improvements in pain, function, and structural integrity of the joint.
IMAGE GUIDED TREATMENTS TO IMPROVE OUTCOMES
At Alleviate, we prioritize precision and accuracy in delivering Platelet-Rich Plasma (PRP) therapy for knee conditions. Our approach involves the utilization of advanced imaging techniques, including fluoroscopy and ultrasound guidance, to ensure optimal placement of PRP and enhance treatment outcomes.
Fluoroscopy-Guided PRP Therapy
Fluoroscopy is a real-time imaging technique that uses continuous X-ray beams to visualize internal structures of the knee joint. It provides dynamic imaging, allowing our medical professionals to monitor the injection process in real-time.
Precise Needle Placement
Fluoroscopy guidance enables our practitioners to accurately position the needle within the target area of the knee joint, ensuring the precise delivery of PRP to the affected tissues.

Visualization of Anatomical Structures
Fluoroscopy provides clear visualization of bony structures, soft tissues, and joint spaces, facilitating the identification of anatomical landmarks and potential areas of pathology within the knee joint.
Real-Time Monitoring
With fluoroscopy, our healthcare providers can monitor the dispersion of PRP within the joint space, ensuring uniform distribution and optimal coverage of the affected areas.

Ultrasound-Guided PRP Therapy
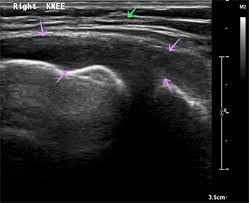
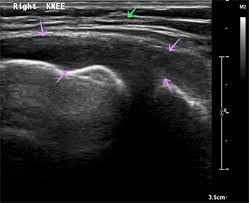
Ultrasound imaging utilizes high-frequency sound waves to create detailed images of soft tissues, including muscles, tendons, ligaments, and synovial structures within
the knee joint.
- Visualization of Soft Tissues: Ultrasound of the knee joint Ultrasound guidance allows for the visualization of soft tissue structures within the knee, including the synovium, menisci, and ligaments, which may be difficult to assess using other imaging modalities.
- Precise Needle Placement: Ultrasound imaging provides real-time visualization of the needle as it enters the knee joint, enabling our practitioners to accurately guide the needle to the target site while avoiding adjacent structures.
- Assessment of Joint Pathology: Ultrasound can help identify areas of joint inflammation, synovial hypertrophy, and cartilage degeneration, providing valuable diagnostic information to guide treatment planning and PRP injection.
In conclusion, precise image-guided PRP therapy utilizing fluoroscopy and ultrasound guidance at
Alleviate Pain Clinic offers patients a state-of-the-art approach to the treatment of knee conditions. By combining advanced imaging technology with expertise in regenerative medicine, we aim to provide our patients with safe, effective, and personalized care to alleviate pain and improve joint function.
References
- Sundman EA, Cole BJ, Fortier LA. Growth factor and catabolic cytokine concentrations are influenced by the cellular composition of platelet-rich plasma. Am J Sports Med. 2011;39(10):2135-2140.
- Anitua E, Sánchez M, Orive G. The importance of understanding what is platelet-rich growth factor (PRGF) and what is not. J Shoulder Elbow Surg. 2011;20(1):e23-4.
- Pierce GF, Mustoe TA, Altrock BW, Deuel TF, Thomason A. Role of platelet-derived growth factor in wound healing. J Cell Biochem. 1991;45(4):319-326.
- Loeser RF. Aging processes and the development of osteoarthritis. Curr Opin Rheumatol. 2013;25(1):108-113.
- Kon E, Filardo G, Delcogliano M, et al. Platelet-rich plasma: new clinical application: a pilot study for treatment of jumper’s knee. Injury. 2009;40(6):598-603.
- Weibrich G, Hansen T, Kleis W, Buch R, Hitzler WE. Effect of platelet concentration in platelet-rich plasma on peri-implant bone regeneration. Bone. 2004;34(4):665-671.
- Alsousou J, Thompson M, Hulley P, Noble A, Willett K. The biology of platelet-rich plasma and its application in trauma and orthopaedic surgery: a review of the literature. J Bone Joint Surg (Br). 2009;91(8):987-996.
- Sánchez M, Anitua E, Azofra J, Aguirre JJ, Andia I. Intra-articular injection of an autologous preparation rich in growth factors for the treatment of knee OA: a retrospective cohort study. Clin Exp Rheumatol. 2008;26(5):910-913.
- Hauser RA, Lackner JB, Steilen-Matias D, Harris DK. A systematic review of dextrose prolotherapy for chronic musculoskeletal pain. Clin Med Insights Arthritis Musculoskelet Disord. 2016;9:139-159.
- Rabago D, Patterson JJ. Prolotherapy: an effective adjunctive therapy for knee osteoarthritis. J Am Osteopath Assoc. 2013;113(2):122-123.
- Smith PA. (2016) Intra-articular Autologous Conditioned Plasma Injections Provide Safe and Efficacious Treatment for Knee Osteoarthritis: An FDA-Sanctioned, Randomized, Double-blind, Placebo-controlled Clinical Trial. The American Journal of Sports Medicine.
- Mishra A, Harmon K, Woodall J, Vieira A. (2011) Sports Medicine Injection Procedures: Platelet-Rich Plasma. Clinics in Sports Medicine.
- Centeno C, Markle J, Dodson E, et al. (2015) The use of biologics in the treatment of the rotator cuff, meniscus, labrum, and other soft tissue injuries. The American Journal of Orthopedics.


 PRP PREPARATION AT ALLEVIATE PAIN CLINIC After centrifugation, the blood separates into three distinct layers:
PRP PREPARATION AT ALLEVIATE PAIN CLINIC After centrifugation, the blood separates into three distinct layers: