Introduction
Frozen shoulder, also known as adhesive capsulitis, is a debilitating musculoskeletal condition characterized by pain and restricted range of motion in the shoulder joint. It is a common condition, affecting approximately 2% to 5% of the general population, with a higher prevalence in individuals aged 40 to 70 years, especially women. Frozen shoulder is a complex and multifactorial disorder that progresses through distinct stages, each with its own set of pathogenic mechanisms, clinical features, symptoms, and treatment approaches. This essay aims to provide a comprehensive overview of the four stages of frozen shoulder, focusing on pathogenesis, clinical features, symptoms, and treatments at each stage.
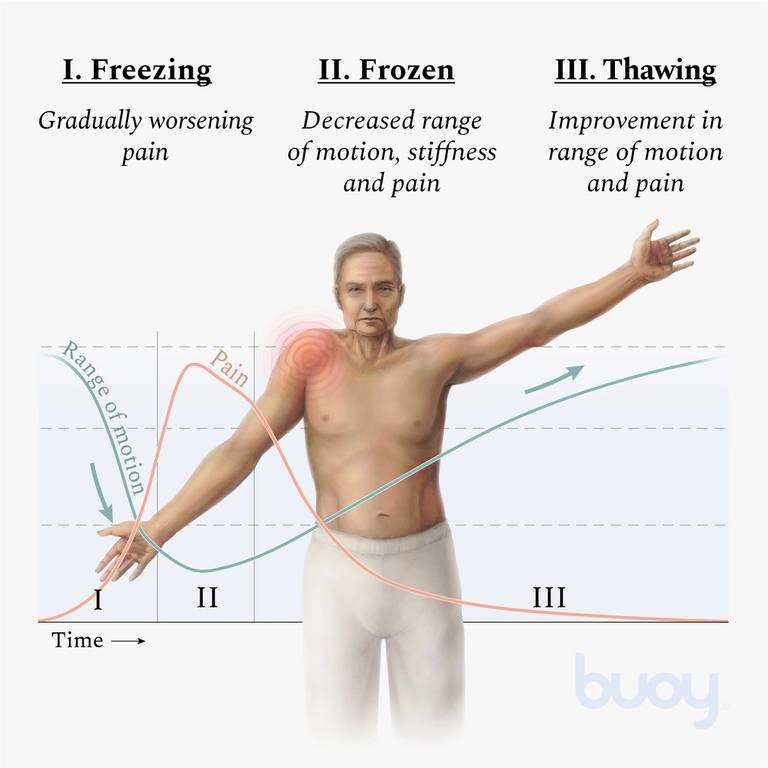
Stage 1 : Pre-freezing or Freezing Stage
Pathogenesis
The pathogenesis of frozen shoulder remains incompletely understood, making it a subject of ongoing research and debate. However, it is generally believed that the condition is multifactorial, with various factors contributing to its development. In the initial stage, known as the pre-freezing or freezing stage, several key pathological processes come into play :
- Synovial inflammation : The condition often begins with inflammation of the synovial membrane lining the joint capsule. This inflammation can be triggered by trauma, microtrauma, or systemic conditions like diabetes mellitus.
- Fibroblast proliferation : As inflammation persists, fibroblasts within the synovium become activated. These fibroblasts play a crucial role in the deposition of collagen, leading to the hallmark feature of frozen shoulder: the thickening and contracture of the joint capsule.
Clinical Features
During the pre-freezing or freezing stage, clinical features are primarily characterized by pain and discomfort in the shoulder joint. These features include:
- Gradual onset of pain : Patients often report a gradual onset of shoulder pain, typically located over the lateral aspect of the upper arm and deltoid region.
- Stiffness and limited range of motion : As fibrosis and contracture of the joint capsule progress, patients experience increasing stiffness in the shoulder joint. Activities such as reaching behind the back or overhead become challenging.
- Pain at night : Many individuals with frozen shoulder experience worsening pain at night, which can disrupt sleep and negatively impact overall quality of life.
Symptoms
The symptoms associated with the pre-freezing or freezing stage are primarily related to pain and stiffness:
- Dull, aching pain in the shoulder that may radiate down the arm.
- Gradual loss of range of motion, especially external rotation and abduction.
- Difficulty with activities of daily living, such as dressing and reaching for objects.
Treatment
Treatment during the pre-freezing stage primarily focuses on pain management and early intervention to prevent progression to the next stages. Common interventions include:
- Analgesics : Non-steroidal anti-inflammatory drugs (NSAIDs) and analgesics can help alleviate pain.
- Physical Therapy : Gentle range of motion exercises and modalities (e.g., heat, ice) may be prescribed to maintain shoulder mobility.
- Corticosteroid Injections : In some cases, corticosteroid injections into the joint can provide relief from pain and inflammation.
- Patient Education : Educating the patient about the condition’s natural course and the importance of adhering to prescribed treatments is crucial.
Stage 2: Frozen Stage
Pathogenesis
The transition from the pre-freezing stage to the frozen stage is marked by a continued progression of fibrosis and contracture within the joint capsule. In this stage, pathogenesis is characterized by:
- Increased collagen deposition : Fibroblasts continue to proliferate and deposit collagen within the joint capsule, leading to further thickening and adhesion.
- Formation of adhesions : As collagen accumulates, adhesions develop between the joint capsule and the humeral head, further restricting movement.
Clinical Features
The frozen stage is characterized by severe limitations in shoulder mobility and persistent pain. Clinical features include:
- Limited range of motion : Patients experience significant restrictions in both active and passive range of motion, with external rotation and abduction being particularly affected.
- Pain at end ranges : Pain is typically elicited when attempting to move the shoulder through its limited range of motion.
- Loss of function : Activities of daily living become increasingly challenging, and patients may require assistance with tasks such as dressing and grooming.
Symptoms
The symptoms of the frozen stage are primarily related to pain and immobility:
- Severe and constant pain in the shoulder.
- Significant loss of range of motion, often described as feeling “frozen” or “locked” in place.
- Impaired function, leading to functional disability.
Treatment
Management of frozen shoulder in this stage is aimed at relieving pain and improving shoulder mobility:
- Physical therapy : Gentle stretching and manual therapy techniques are used to gradually improve range of motion. Therapists may also employ modalities such as ultrasound or heat to aid in relaxation.
- Corticosteroid injections : In some cases, corticosteroid injections into the joint capsule can provide short-term pain relief.
- Hydrodilatation: A procedure in which sterile water is injected into the joint capsule to stretch it, relieving some of the stiffness.
- Home exercises : Patients are often given specific exercises to perform at home to maintain and improve shoulder mobility.
- Patient education : Patients should be educated about the importance of compliance with therapy and exercises, as well as realistic expectations for recovery.
Stage 3 : Thawing Stage
Pathogenesis
The thawing stage represents a phase of gradual improvement in shoulder mobility. While the exact mechanisms underlying this stage are not fully understood, it is believed that the gradual breakdown of adhesions and collagen deposition leads to increased flexibility.
Clinical Features
During the thawing stage, patients begin to experience a gradual improvement in shoulder mobility. Clinical features include:
- Slowly improving range of motion : Patients may notice a gradual increase in their ability to move the shoulder joint.
- Decreased pain : Pain levels tend to decrease as mobility improves, although discomfort may still be present during certain movements.
- Continuing functional improvement : Patients regain the ability to perform some daily tasks that were previously difficult or impossible.
Symptoms
Symptoms during the thawing stage are marked by a gradual reduction in pain and improved mobility:
- Reduced shoulder pain, especially at rest.
- Gradual restoration of range of motion, allowing for improved function.
Treatment
Management during the thawing stage focuses on maximizing gains in shoulder mobility and function:
- Continued physical therapy : Patients continue with stretching and strengthening exercises to further improve range of motion and shoulder function.
- Pain management : While pain tends to decrease naturally during this stage, some patients may benefit from over-the-counter pain relievers or occasional corticosteroid injections if pain persists.
- Patient education : Reinforcing the importance of ongoing exercises and gradual improvements in function is crucial to maintain motivation and adherence to the treatment plan.
Stage 4 : Recovery Stage
Pathogenesis
The recovery stage represents the final phase of frozen shoulder, characterized by the gradual resolution of symptoms and the return of near-normal shoulder function. Pathogenesis in this stage involves the continued breakdown of collagen adhesions and the restoration of joint homeostasis.
Clinical Features
The primary clinical feature of the recovery stage is the near-complete restoration of shoulder function:
- Subsiding pain : Pain levels continue to decrease, and many patients experience minimal to no pain during daily activities.
- Full or near-full range of motion : Patients regain the ability to move their shoulder through a full range of motion, allowing them to perform most activities without difficulty.
- Improved quality of life : Patients experience a significant improvement in their overall quality of life as they regain the ability to engage in routine activities without limitation.
Symptoms
Symptoms in the recovery stage are minimal and primarily related to residual discomfort :
- Occasional mild discomfort or soreness.
- Complete or near-complete restoration of shoulder function.
Treatment
Treatment during the recovery stage primarily involves monitoring and reassurance:
- Periodic follow-up : Patients may have occasional check-ups with their healthcare provider to monitor progress and address any residual symptoms.
- Maintenance exercises : Patients are encouraged to continue with maintenance exercises to preserve shoulder mobility and strength.
- Lifestyle modifications : Patients are advised to maintain a healthy lifestyle and avoid activities that could potentially lead to shoulder injuries or recurrences.
Conclusion
Frozen shoulder is a challenging musculoskeletal condition that progresses through four distinct stages, each with its own pathogenesis, clinical features, symptoms, and treatment strategies. Understanding these stages is crucial for healthcare providers and patients, as it guides the management and expectations throughout the course of the condition. Early intervention and appropriate treatment can significantly improve outcomes, helping patients regain optimal shoulder function and quality of life. While the pathogenesis of frozen shoulder remains the subject of ongoing research, a multidisciplinary approach that includes physical therapy, pain management, and patient education is essential to effectively address this debilitating condition.
References
- Mezian K, Coffey R, Chang KV. Frozen Shoulder. [Updated 2022 Aug 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/ books/ NBK482162/
- Dias R, Cutts S, Massoud S. Frozen shoulder. BMJ. 2005 Dec 17;331(7530):1453-6. doi: 10.1136/bmj.331.7530.1453. PMID: 16356983; PMCID: PMC1315655.
- Image taken from https://www.buoyhealth.com/ learn/frozen-shoulder#symptoms
- Image taken from https://www.richmondrehab.com.au/ blog/ physiotherapy / frozen-shoulder