Introduction
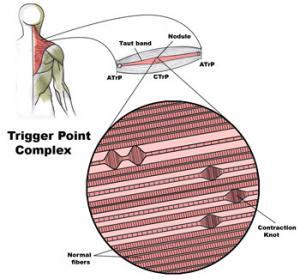
The mystique surrounding trigger points, those elusive knots of muscle fibers responsible for unexplained pain, has puzzled both patients and healthcare professionals for years. While their existence can be felt through palpation, the true nature and precise location of trigger points have often remained hidden. In this in-depth exploration, we delve into the potential game-changer in the diagnosis and treatment of trigger points – ultrasound.
Trigger Points Unveiled: A Brief
Overview
Before we embark on our journey into the world of ultrasound and trigger points, it’s essential to understand what trigger points are. These hyperirritable bundles or nodules of muscle fibers, often firmer than the surrounding tissue, have been responsible for chronic pain conditions in countless individuals. The traditional approach to identifying them has largely relied on palpation.
Can Ultrasound Solve the Mystery of Trigger Points?
Direct Visualization of Trigger Points
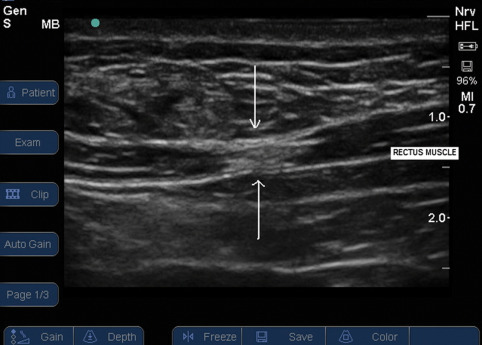
Trigger point visualised on Ultrasound
Early attempts to confirm the presence of myofascial trigger points using imaging, such as magnetic resonance elastography, showed promise but were not widely adopted. However, recent advancements in ultrasound have provided new hope.
Sikdar et al. have successfully utilized ultrasound to visualize and characterize trigger points. These trigger points appear as focal, hypoechoic (darker) regions with an elliptical shape, measuring approximately 0.16 cm. This breakthrough suggests that ultrasound could offer a more objective diagnosis of trigger points.
Injection of Peripheral Nerves
Trigger point injections have played a pivotal role in managing various conditions, including headache, low back pain, and musculoskeletal disorders. Some of these injections target nerves supplying specific regions, shedding light on the role of peripheral nerves in trigger point-related pain.
Greater Occipital Nerve
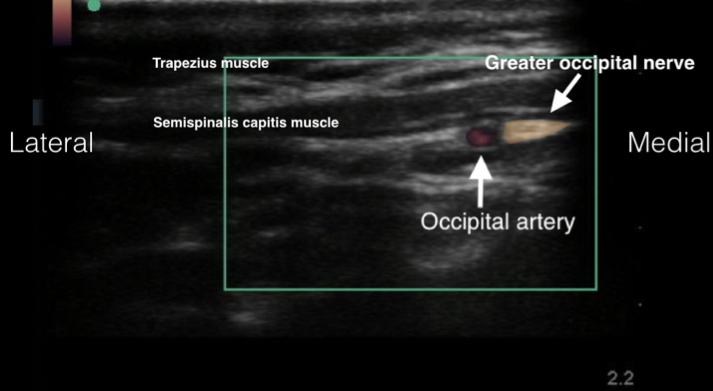
The greater occipital nerve entrapment is often linked to cervicogenic headaches. This nerve entrapment’s referral pattern coincides with that of trigger points, suggesting a potential connection. Ultrasound-guided blockade techniques for the greater occipital nerve have emerged as a valuable tool in headache management.
Abdominal Cutaneous Nerve
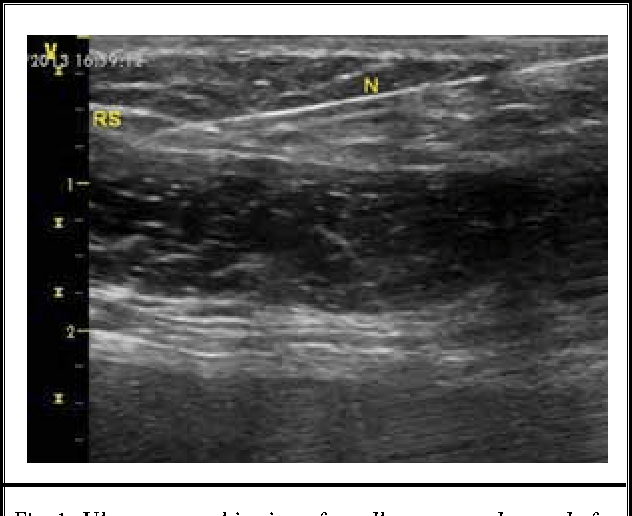
Trigger points in the abdominal wall have been associated with lower abdominal pain, potentially caused by entrapped cutaneous nerves. Ultrasound-guided blocks, such as the ilioinguinal and iliohypogastric nerve blocks, have proven effective in managing lower abdominal pain.
Dorsal Ramus of Spinal Nerve
Chronic low back pain, often challenging to diagnose precisely, has responded to trigger point injections. CT-guided dorsal ramus block has demonstrated efficacy in treating myofascial low back pain, hinting at the possibility of nerve injections playing a role in pain relief.
Lumbar Plexus
Case reports suggest that trigger point injections could relieve pain in remote areas. These injections may inadvertently affect the lumbar plexus, leading to pain relief. Ultrasound-guided lumbar plexus blocks offer a promising avenue for targeted pain management.
Pudendal Nerve
Intriguingly, trigger point injections in the levator ani muscles have proven effective in managing chronic pelvic pain. This effect may be attributed to concomitant pudendal nerve blocks. Ultrasound-guided pudendal nerve blocks via the transgluteal approach have become a valuable technique in pelvic pain management.
Other Advantages of Ultrasound in Trigger Point Injections
Beyond its role in visualizing trigger points and guiding nerve injections, ultrasound offers several additional advantages in trigger point therapy. These include:
- Reduced Risk of Complications : Serious complications associated with trigger point injections, though rare, can be minimized with direct visualization of surrounding tissues and structures.
- Real-time Imaging : Ultrasound enables real-time monitoring of injectate spread around relevant structures, increasing the accuracy and success rate of injections.
Conclusion
Ultrasound’s emergence as a diagnostic and therapeutic tool in the realm of trigger points is reshaping how we approach these enigmatic sources of chronic pain. With the ability to visualize trigger points directly, guide precise injections to target nerves, and reduce the risk of complications, ultrasound is revolutionizing trigger point diagnosis and treatment.
We At ALLEVIATE continuously strive to uncover the intricacies of trigger points and ultrasound technology advances, the future holds promise for improved pain management and enhanced patient outcomes. The collaboration between healthcare professionals and ultrasound technology offers hope to those who have long grappled with the mysteries of trigger points, bringing them into clearer focus and providing relief from persistent pain.
References
- Simons DG. New views of myofascial trigger points: etiology and diagnosis. Archives of Physical Medicine and Rehabilitation. 2008;89(1):157–159. [PubMed] [Google Scholar]
- Lewis J, Tehan P. A blinded pilot study investigating the use of diagnostic ultrasound for detecting active myofascial trigger points. 1999;79(1):39–44. [PubMed] [Google Scholar]
- Sikdar S, Shah JP, Gebreab T, et al. Novel applications of ultrasound technology to visualize and characterize myofascial trigger points and surrounding soft tissue. Archives of Physical Medicine and Rehabilitation. 2009;90(11):1829–1838. [PMC free article] [PubMed] [Google Scholar]
- Botwin KP, Sharma K, Saliba R, Patel BC. Ultrasound-guided trigger point injections in the cervicothoracic musculature: a new and unreported technique. Pain Physician. 2008;11(6):885–889. [PubMed] [Google Scholar]
- Janis JE, Hatef DA, Reece EM, McCluskey PD, Schaub TA, Guyuron B. Neurovascular compression of the greater occipital nerve: implications for migraine headaches. Plastic and Reconstructive Surgery. 2010;126(6):1996–2001. [PubMed] [Google Scholar]
- Blumenfeld A, Ashkenazi A. Nerve blocks, trigger point injections and headache. 2010;50(6):953–954. [PubMed] [Google Scholar]
- Blumenfeld A, Ashkenazi A, Grosberg B, et al. Patterns of use of peripheral nerve blocks and trigger point injections among headache practitioners in the USA: results of the American headache society interventional procedure survey (AHS-IPS) 2010;50(6):937–942. [PubMed] [Google Scholar]
- Ashkenazi A, Young WB. The effects of greater occipital nerve block and trigger point injection on brush allodynia and pain in migraine. 2005;45(4):350–354. [PubMed] [Google Scholar]
- Greher M, Moriggl B, Curatolo M, Kirchmair L, Eichenberger U. Sonographic visualization and ultrasound-guided blockade of the greater occipital nerve: a comparison of two selective techniques confirmed by anatomical dissection. British Journal of Anaesthesia. 2010;104(5):637–642. [PubMed] [Google Scholar]
- Narouze S, editor. Atlas of Ultrasound-Guided Procedures in Interventional Pain Management.New York, NY, USA: Springer; 2011. [Google Scholar]
- Kuan LC, Li YT, Chen FM, Tseng CJ, Wu SF, Kuo TC. Efficacy of treating abdominal wall pain by local injection. Taiwanese Journal of Obstetrics and Gynecology. 2006;45(3):239–243. [PubMed] [Google Scholar]
- Whiteside JL, Barber MD, Walters MD, Falcone T, Morse A. Anatomy of ilioinguinal and iliohypogastric nerves in relation to trocar placement and low transverse incisions. American Journal of Obstetrics and Gynecology. 2003;189(6):1574–1578. [PubMed] [Google Scholar]
- Peleg R, Gohar J, Koretz M, Peleg A. Abdominal wall pain in pregnant women caused by thoracic lateral cutaneous nerve entrapment. European Journal of Obstetrics Gynecology. 1997;74(2):169–171. [PubMed] [Google Scholar]
- Lim SL, Ng S, Tan GM. Ilioinguinal and iliohypogastric nerve block revisited: single shot versus double shot technique for hernia repair in children. Paediatric Anaesthesia. 2002;12(3):255–260. [PubMed] [Google Scholar]
- Oriola F, Toque Y, Mary A, Gagneur O, Beloucif S, Dupont H. Bilateral ilioinguinal nerve block decreases morphine consumption in female patients undergoing nonlaparoscopic gynecologic surgery. Anesthesia and Analgesia. 2007;104(3):731–734. [PubMed] [Google Scholar]
- Aveline C, Le Hetet H, Le Roux A, et al. Comparison between ultrasound-guided transversus abdominis plane and conventional ilioinguinal/iliohypogastric nerve blocks for day-case open inguinal hernia repair. British Journal of Anaesthesia. 2011;106(3):380–386. [PubMed] [Google Scholar]
- Chiono J, Bernard N, Bringuier S, et al. The ultrasound-guided transversus abdominis plane block for anterior iliac crest bone graft postoperative pain relief: a prospective descriptive study. Regional Anesthesia and Pain Medicine. 2010;35(6):520–524. [PubMed] [Google Scholar]
- Baaj JM, Alsatli RA, Majaj HA, Babay ZA, Thallaj AK. Efficacy of ultrasound-guided transversus abdominis plane (TAP) block for post-cesarean section delivery analgesia—a double-blind, placebo-controlled, randomized study. Middle East Journal of Anesthesiology. 2010;20(6):821–826. [PubMed] [Google Scholar]
- Ra YS, Kim CH, Lee GY, Han JI. The analgesic effect of the ultrasound-guided transverse abdominis plane block after laparoscopic cholecystectomy. Korean Journal of Anesthesiology. 2010;58(4):362–368. [PMC free article] [PubMed] [Google Scholar]
- Eichenberger U, Greher M, Kirchmair L, Curatolo M, Moriggl B. Ultrasound-guided blocks of the ilioinguinal and iliohypogastric nerve: accuracy of a selective new technique confirmed by anatomical dissection. British Journal of Anaesthesia. 2006;97(2):238–243. [PubMed] [Google Scholar]
- Chan V, Abbas S, Brull R, Moriggl B, Perlas A. Ultrasound Imaging for Regional Anesthesia—A Practical Guide. 3rd edition. Vincent Chan; 2010. [Google Scholar]
- Miyakoshi N, Shimada Y, Kasukawa Y, Saito H, Kodama H, Itoi E. Total dorsal ramus block for the treatment of chronic low back pain: a preliminary study. Joint Bone Spine. 2007;74(3):270–274. [PubMed] [Google Scholar]
- Greher M, Kirchmair L, Enna B, et al. Ultrasound-guided lumbar facet nerve block: accuracy of a new technique confirmed by computed tomography. 2004;101(5):1195–1200. [PubMed] [Google Scholar]
- Iguchi M, Katoh Y, Koike H, Hayashi T, Nakamura M. Randomized trial of trigger point injection for renal colic. International Journal of Urology. 2002;9(9):475–479. [PubMed] [Google Scholar]
- Langford CF, Nagy SU, Ghoniem GM. Levator ani trigger point injections: an underutilized treatment for chronic pelvic pain. Neurourology and Urodynamics. 2007;26(1):59–62. [PubMed] [Google Scholar]
- Nelson LS, Hoffman RS. Intrathecal injection: unusual complication of trigger-point injection therapy. Annals of Emergency Medicine. 1998;32(4):506–508. [PubMed] [Google Scholar]
- Image taken from @article{Batistaki2013UltrasoundguidedAA, title={Ultrasound-guided anterior abdominal cutaneous nerve block for the management of bilateral abdominal cutaneous nerve entrapment syndrome (ACNES).}, author={Chrysanthi Batistaki and Theodosios Saranteas and Areti Adoni and Georgia Kostopanagiotou}, journal={Pain physician} year={2013}, volume={16 6}, pages={ E799-801
- Image taken from https://med.emory.edu/departments/emergency-medicine/sections/ultrasound/case-of-the-month/procedures/occipital-nerve-block.html
- Trigger point visualised on Ultrasound. Image taken from https://www.bjanaesthesia.org.uk/article/S0007-0912%2817%2933096-9/fulltext