Introduction
Craniocervical instability (CCI) is a condition that affects the stability of the connection between the skull and the upper spine, leading to a range of symptoms and potential impacts on an individual’s quality of life. In this comprehensive blog, we will delve into the causes of craniocervical instability, identify common symptoms, explore the impact on daily life, discuss the challenges of diagnosis, and highlight innovative treatments, with a special focus on image-guided stem cells, Platelet-Rich Plasma (PRP), and Prolotherapy treatments for Craniocervical instability.
What are the causes of Craniocervical Instability?
CCI) is a condition characterized by abnormal movement or instability between the skull and the upper cervical spine. Several factors can contribute to the development of craniocervical instability, and it often results from a combination of these factors. The primary causes of craniocervical instability include:
- Ligament Laxity : One of the leading causes of CCI is laxity or weakness in the ligaments that support the craniocervical junction. Ligaments play a crucial role in stabilizing the spine, and if they become lax or damaged, it can lead to excessive movement between the skull and the upper cervical vertebrae.
- Trauma : Physical trauma, particularly injuries that involve the head and neck, can contribute to craniocervical instability. Whiplash injuries, which commonly occur in motor vehicle accidents, can damage ligaments and disrupt the normal biomechanics of the craniocervical junction.
- Congenital Abnormalities : Some individuals may be predisposed to craniocervical instability due to congenital abnormalities in the structure of the cervical spine or skull. These abnormalities may affect the alignment and stability of the craniocervical junction from birth.
- Connective Tissue Disorders : Conditions that affect connective tissues, such as Ehlers-Danlos syndrome, can contribute to ligament laxity throughout the body, including the craniocervical region. Connective tissue disorders can weaken the structural integrity of the ligaments, making them more prone to instability.
- Degenerative Changes : Aging and degenerative changes in the cervical spine can also play a role in the development of craniocervical instability. Over time, wear and tear on the spine can lead to changes in the vertebral discs, joints, and ligaments, contributing to instability.
- Inflammatory Conditions : Inflammatory conditions affecting the cervical spine, such as rheumatoid arthritis, can lead to joint damage and ligament instability. Inflammation can weaken the supportive structures in the craniocervical junction, contributing to instability.
What are the symptoms of Craniocervical Instability?
Craniocervical instability (CCI) can manifest with a variety of symptoms due to the abnormal movement or instability between the skull and the upper cervical spine. It’s important to note that the severity and combination of symptoms can vary among individuals. Here are 12 common symptoms associated with craniocervical instability:
- Neck Pain : Persistent and often severe neck pain is a hallmark symptom of CCI. The instability and abnormal movement in the craniocervical region can lead to chronic discomfort.
- Headaches : Individuals with CCI often experience chronic headaches, which may range from tension-type headaches to more severe migraines. The instability can contribute to increased pressure and pain.
- Dizziness and Vertigo : Instability in the craniocervical junction can result in feelings of dizziness and vertigo. Changes in head position may trigger these symptoms.
- Nausea and Vomiting : Some individuals with CCI may experience nausea and vomiting, particularly during episodes of instability. This can be a result of the impact on the vestibular system.
- Tinnitus : Ringing or buzzing in the ears (tinnitus) can be associated with craniocervical instability, possibly due to changes in blood flow or pressure within the head.
- Visual Disturbances : Craniocervical instability may cause visual disturbances, including blurred vision, light sensitivity, and difficulty focusing.
- Facial Pain : Pain in the face, especially around the jaw and temporal regions, can be a symptom of CCI. This may be related to nerve compression or irritation.
- Difficulty Swallowing : Instability in the craniocervical region can affect the muscles involved in swallowing, leading to difficulty or discomfort while swallowing.
- Cognitive Dysfunction : Some individuals with CCI report cognitive dysfunction, including issues with concentration, memory, and overall mental clarity.
- Fatigue : Chronic fatigue is a common complaint among individuals with craniocervical instability. The persistent pain and neurological symptoms can contribute to a sense of exhaustion.
- Sleep Disturbances : Sleep disruptions, including difficulty falling asleep and staying asleep, may be associated with the discomfort and pain caused by craniocervical instability.
- Mood Changes : Anxiety and depression may be linked to the impact of craniocervical instability on daily life. The chronic nature of the condition and its effects on physical and mental well-being can contribute to mood changes.
Pathogenesis of the symptoms of Craniocervical Instability
The pathogenesis of symptoms in craniocervical instability (CCI) involves abnormal movement and instability in the region where the skull meets the upper cervical spine. This instability can lead to compression, irritation, or dysfunction of various structures, resulting in a range of symptoms. Let’s explore how these symptoms arise due to compression or dysfunction of specific structures:

Compression of Spinal Cord or Nerve Roots
- Pathogenesis : Instability in the craniocervical junction can result in abnormal movement, leading to compression of the spinal cord or nerve roots.
- Resultant Symptoms :
- Persistent neck pain
- Radiating pain into the arms
- Numbness or tingling in the extremities
Brainstem Compression
- Pathogenesis: Instability may cause compression of the brainstem, a critical structure that connects the brain to the spinal cord.
- Resultant Symptoms :
- Dizziness
- Vertigo
- Difficulty with balance and coordination
- Visual disturbances
Vascular Compression
- Pathogenesis: Compression of blood vessels in the craniocervical region can affect blood flow to the brain.
- Resultant Symptoms :
- Headaches, including migraines
- Tinnitus (ringing in the ears)
- Cognitive dysfunction
Compression of Cranial Nerves
- Pathogenesis: Instability may lead to compression of cranial nerves, particularly those responsible for facial sensation and movement.
- Resultant Symptoms :
- Facial pain
- Abnormalities in facial sensation
- Difficulty swallowing
Impact on Ligaments and Muscles
- Pathogenesis: Ligament laxity and muscle strain due to instability can contribute to overall dysfunction in the craniocervical region.
- Resultant Symptoms :
- Neck stiffness
- Limited range of motion
- Muscular pain and spasms
Nerve Impingement
- Pathogenesis: Abnormal movement may lead to nerve impingement, causing irritation and dysfunction.
- Resultant Symptoms :
- Shooting pain along the spine
- Radicular pain radiating into the limbs
- Muscle weakness
Impact on Cerebrospinal Fluid Flow
- Pathogenesis: Instability may alter the normal flow of cerebrospinal fluid in the spinal canal.
- Resultant Symptoms :
- Headaches, often exacerbated by changes in position
- Increased intracranial pressure
Connective Tissue Strain
- Pathogenesis: Instability can strain the connective tissues, including ligaments and fascia.
- Resultant Symptoms :
- Increased joint laxity
- Generalized pain and discomfort
Inflammatory Responses
- Pathogenesis: Chronic irritation and compression can trigger inflammatory responses.
- Resultant Symptoms :
- Swelling in the affected area
- Increased pain and tenderness
Impact on Cervical Joints
- Pathogenesis: Abnormal movement can affect the cervical joints.
- Resultant Symptoms :
- Joint pain
- Crepitus (crackling or popping sounds with movement)
Understanding the pathogenesis of symptoms in CCI involves recognizing how the instability affects specific structures in the craniocervical region. The variety of symptoms observed reflects the complex interplay between the nervous system, vascular structures, and supporting tissues. It’s important to emphasize that these symptoms can vary in intensity and may not be present in every individual with CCI. Additionally, the symptoms of craniocervical instability can overlap with other medical conditions, making an accurate diagnosis crucial for effective management.
How do you diagnose Craniocervical Instability?
Diagnosing craniocervical instability (CCI) can indeed be challenging, and patients often face the frustration of multiple doctor visits with inconclusive findings on standard imaging studies like MRI. Given the dynamic nature of the instability, relying solely on static images may not capture the full extent of the problem. Here are some key investigations, including the use of dynamic X-rays, that can be valuable in the diagnosis of craniocervical instability:
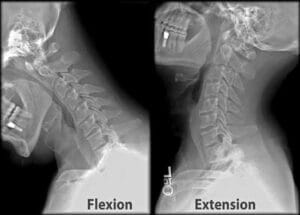
Dynamic X-Rays (Flexion and Extension Views)
Dynamic X-rays involve taking images of the cervical spine while the patient moves their head in flexion (forward bending) and extension (backward bending). These views can reveal abnormal movement, misalignments, or instability that may not be apparent on static images like MRIs. For individuals with CCI, dynamic X-rays are often more indicative of the condition.
CT (Computed Tomography) Scan
CT scans can provide detailed images of the bones and joints in the craniocervical region. While they may not show soft tissues as well as an MRI, CT scans can reveal bony abnormalities, fractures, or signs of instability.
Cine MRI
Unlike traditional MRIs, cine MRI captures dynamic images of the spine in motion. This can be particularly useful in identifying abnormal movement or instability. It allows the healthcare provider to visualize changes in real-time, enhancing diagnostic accuracy.

Digital Motion X-ray (DMX)
Digital Motion X-ray is a specialized imaging technique that captures dynamic images of the spine during movement. It is especially useful for assessing instability and abnormal motion in the cervical spine.
Upright MRI
Traditional MRI scans are performed with the patient lying down, which may not replicate the conditions that cause symptoms in individuals with CCI. Upright MRI allows imaging in weight-bearing positions, providing a more accurate representation of the spine’s condition during daily activities.
Neurological and Orthopedic Evaluation
A thorough clinical assessment by a neurologist or orthopedic specialist is crucial. They will evaluate symptoms, perform neurological examinations, and consider the patient’s medical history to guide further diagnostic steps.
Dynamic CT Myelogram
In some cases, a dynamic CT myelogram may be conducted. This involves injecting contrast dye into the spinal canal before obtaining CT images. It can provide detailed information about the spinal cord and nerve roots.
Blood Tests
While not directly diagnostic of CCI, blood tests may be conducted to rule out other potential causes of symptoms, such as inflammatory or autoimmune conditions.For a patient with craniocervical instability who may be experiencing symptoms like depression due to the chronic nature of their condition, a collaborative approach involving mental health professionals is also crucial. Addressing the emotional well-being of the patient is an integral part of comprehensive care.
It’s important for individuals experiencing symptoms of craniocervical instability to work closely with healthcare professionals who specialize in spine disorders. A multi-disciplinary approach, involving specialists in neurology, orthopedics, and radiology, is often necessary to reach an accurate diagnosis and develop an effective treatment plan.
What are the treatment options for Craniocervical Instability?
The treatment of craniocervical instability (CCI) often involves a comprehensive and multidisciplinary approach. While there is no one-size-fits-all solution, innovative therapies such as image-guided stem cell therapy, Platelet-Rich Plasma (PRP), and prolotherapy have shown promise in addressing the underlying causes and providing relief for individuals with CCI.
Conservative Measures
- Physical Therapy: Tailored physical therapy programs can help improve cervical stability, strengthen supporting muscles, and enhance range of motion.
- Cervical Collars: Temporary use of cervical collars may provide support and restrict excessive movement during the healing process.
Medications
- Anti-Inflammatory Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to manage pain and inflammation.
Interventional Pain Management
- Cervical Facet Joint Injections: These injections can help alleviate pain by targeting specific nerves in the cervical spine.
- Stem Cell Therapy: Image-guided stem cell therapy involves injecting stem cells, often derived from the patient’s own body (autologous), into the affected ligaments and tissues. The goal is to promote tissue regeneration, reduce inflammation, and enhance stability. Advanced imaging techniques, such as fluoroscopy or ultrasound, guide the precise placement of stem cells.
- Platelet-Rich Plasma (PRP): PRP therapy utilizes the patient’s own concentrated platelets, which are rich in growth factors, to stimulate healing and tissue repair. Like stem cell therapy, image guidance ensures accurate injection placement.
- Prolotherapy Injections: Prolotherapy involves injecting a solution (often containing dextrose or other irritants) into the affected ligaments. This stimulates the body’s natural healing response, promoting the formation of new, stronger tissue. Image guidance ensures targeted delivery of the solution to the specific areas of instability.
Surgical Options
- In some cases, when conservative measures and injections do not provide sufficient relief, surgical intervention may be considered. Surgical options may include stabilization procedures, fusion, or other techniques aimed at addressing the underlying instability.
Lifestyle Modifications
- Patients may benefit from adopting lifestyle modifications to reduce strain on the craniocervical junction. This may include avoiding activities that exacerbate symptoms and maintaining good posture.
Psychotherapy and Support
- Chronic conditions like CCI can impact mental health. Psychotherapy and support groups can provide emotional support and coping strategies.
Regular Monitoring and Adjustments
- Treatment plans for CCI may need adjustments based on the individual’s response and evolving symptoms. Regular follow-up with healthcare providers is essential for ongoing assessment and modification of the treatment approach.
Before pursuing any treatment, individuals with CCI should consult with a healthcare professional who specializes in spine disorders. The provider can conduct a thorough evaluation, including imaging studies, to determine the most appropriate and effective course of action. The goal of treatment is not only to alleviate symptoms but also to address the root causes of craniocervical instability and improve overall quality of life.
What is the impact of craniocervical instability on the quality of life?
Craniocervical instability (CCI) can have a significant and varied impact on an individual’s quality of life. The severity of symptoms and their implications for daily functioning can vary widely from person to person. Here are several ways in which CCI can affect the quality of life:
Chronic Pain
- Description: Persistent neck pain and headaches are common symptoms of CCI.
- Impact: Chronic pain can limit mobility, hinder daily activities, and affect overall well-being.
Neurological Symptoms
- Description: Symptoms such as dizziness, vertigo, visual disturbances, and cognitive dysfunction.
- Impact: Neurological symptoms can impact concentration, memory, and the ability to perform tasks requiring focus.
Functional Limitations
- Description: Instability may result in limitations in neck movement and overall functional capacity.
- Impact: Reduced ability to perform activities of daily living, including work-related tasks and recreational activities.
Emotional Well-being
- Description: Living with a chronic condition can contribute to emotional distress, including anxiety and depression.
- Impact: Emotional well-being may be affected due to the challenges of managing symptoms and uncertainty about the future.
Social Impact
- Description: Chronic pain and neurological symptoms may limit social interactions and participation in social activities.
- Impact: Individuals with CCI may experience social isolation, impacting their overall quality of life.
Sleep Disturbances
- Description: Pain and discomfort may lead to difficulties in falling asleep and staying asleep.
- Impact: Sleep disturbances can contribute to fatigue, exacerbating the overall impact on daily functioning.
Impact on Work
- Description: Symptoms may affect the ability to work, leading to productivity challenges and potential employment issues.
- Impact: Work-related stress, absenteeism, and decreased job satisfaction may occur.
Treatment Burden
- Description: The need for ongoing medical appointments, treatments, and interventions.
- Impact: Managing CCI often involves a complex treatment regimen, impacting the individual’s time and financial resources.
Uncertainty and Anxiety
- Description: The chronic and sometimes unpredictable nature of CCI may contribute to anxiety about the future.
- Impact: Uncertainty regarding symptom progression and the effectiveness of treatments can affect mental well-being.
Coping with Limitations
- Description: Learning to cope with physical limitations and adapting to lifestyle changes.
- Impact: Adjusting to life with CCI may require developing new coping strategies and finding ways to maintain a sense of normalcy.
Impact on Relationships
- Description: Changes in physical and emotional well-being can impact relationships with family and friends.
- Impact: Supportive relationships are crucial, but adjustments may be necessary to accommodate the challenges posed by CCI.
Potential for Disability
- Description: In severe cases, the impact of CCI may lead to disability.
- Impact: Disability can significantly alter an individual’s lifestyle, requiring additional support and accommodations.
It’s important to recognize that the impact of CCI is multifaceted, affecting physical, emotional, social, and occupational aspects of an individual’s life. A comprehensive and patient-centered approach to managing CCI involves addressing not only the physical symptoms but also the emotional and social challenges that accompany the condition. Seeking support from healthcare professionals, such as at Alleviate Pain Clinic including who can help individuals develop tailored strategies incorporating regenerative injection treatments combined with a focussed multidisciplinary approach to enhance their quality of life despite the challenges posed by CCI





