Introduction
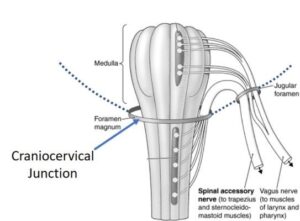
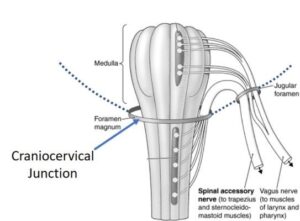
The vagus nerve, also known as the wandering nerve, is one of the longest and most complex nerves in the body. It plays a vital role in regulating numerous bodily functions, including heart rate, digestion, and immune response. While the vagus nerve’s primary course is through the neck, it is not immune to the impact of cervical instability a condition that can lead to compression or irritation of the nerve. This article explores the intriguing relationship between cervical instability and vagus nerve symptoms, shedding light on the potential consequences and treatment options.The Vagus nerve originates in the brainstem, traveling down through the neck (external to the spinal cord and spine). Since it travels outside the spinal cord, it is exposed to potential muscular, fascial, or structural entrapment.


Understanding Cervical Instability
Cervical instability, as the term suggests, refers to excessive motion or instability in the cervical spine (neck). It typically involves the misalignment of cervical vertebrae or damage to the ligaments and supporting structures that keep the neck stable. This instability can lead to a range of symptoms, including pain, limited range of motion, and neurological deficits. In patients suffering with craniocervical instability,the skull is not stable on the neck. So these nerves are bound to get more irritated and even compressed at times,leading to irritation and vagus nerve dysfunction.
The Vagus Nerve: An Overview
The vagus nerve, the tenth cranial nerve, has a vast reach within the body, influencing multiple systems and functions. It is responsible for:
- Heart Rate Regulation : The vagus nerve helps maintain a healthy heart rate by slowing it down when necessary.
- Digestive Function : It plays a crucial role in digestion, stimulating stomach acid production and promoting gastrointestinal motility.
- Immune Response : The vagus nerve is involved in modulating the body’s immune response to infections and inflammation.
- Inflammation Control : It helps regulate the body’s inflammatory responses, potentially impacting various chronic conditions.
Given the vagus nerve’s extensive reach and influence, any interference or irritation can result in a wide range of symptoms.
The Connection: Cervical Instability and Vagus Nerve Symptoms
Recent research and clinical observations have shed light on the link between cervical instability and vagus nerve symptoms. It is believed that the instability in the cervical spine can lead to compression, irritation, or tension on the vagus nerve, resulting in various symptoms. Some of the common vagus nerve-related symptoms associated with cervical instability include:
- Dysautonomia : Dysautonomia is a condition where the autonomic nervous system, which is partially regulated by the vagus nerve, malfunctions. Symptoms can include rapid heart rate, blood pressure fluctuations, and digestive issues.
- Chronic Fatigue : Compression or irritation of the vagus nerve can lead to chronic fatigue, a debilitating condition characterized by extreme tiredness.
- Digestive Problems : Gastroparesis, characterized by delayed stomach emptying, and irritable bowel syndrome (IBS) are potential digestive issues linked to vagus nerve dysfunction.
- Inflammatory Conditions : Dysregulation of the vagus nerve can exacerbate inflammation in the body, potentially contributing to various inflammatory conditions.
- Neurological Symptoms : These may include headaches, dizziness, and difficulty concentrating.
Research and Evidence
- Hauser : In his work Dr Hauser of Caring Medical discusses the impact of cervical instability on the vagus nerve and presents cases where patients with vagus nerve-related symptoms experienced relief after undergoing prolotherapy, a regenerative treatment that strengthens the affected ligaments and stabilizes the cervical spine.
- Gillick et al. (2015) : The study by Gillick and colleagues reviews the role of surgery in addressing cervical spine issues in rheumatoid arthritis. While it does not directly explore the vagus nerve’s involvement, it highlights the significance of addressing cervical spine problems in conditions that can potentially affect the vagus nerve.
- Neurologic-Like Symptoms and Conditions : Studies also discuss how cervical spine instability can mimic neurological conditions, further highlighting the complexity of this issue.
Treatment Options
- Prolotherapy : Prolotherapy has shown great promise in stabilizing the cervical spine and alleviating symptoms related to vagus nerve dysfunction caused by cervical instability.
- Physical Therapy : Targeted exercises and therapies can help strengthen neck muscles, improve posture, and potentially reduce cervical instability.
- Surgery : In severe cases where conservative treatments fail, surgical intervention to address cervical instability may be considered.
Conclusion
The connection between cervical instability and vagus nerve symptoms is a compelling area of research and clinical observation. While further studies are needed to fully understand the mechanisms and relationships at play, the evidence suggests that cervical instability can indeed impact the vagus nerve, leading to a wide array of symptoms. Identifying and addressing cervical instability through treatments like prolotherapy and physical therapy may offer relief to those experiencing vagus nerve-related symptoms. As our understanding of this connection deepens, it opens new avenues for improving the quality of life for individuals facing these challenging conditions.
References
Images taken from https://tao-fit.com/vagus-nerve-entrapment/
Images taken from https://regenexx.com/blog/vagus-nerve-and-neck-pain/



