Introduction
Knee pain is a common ailment that can significantly impact one’s quality of life. Understanding the underlying causes of knee pain is crucial for accurate diagnosis and effective treatment. Two conditions often associated with knee pain are Chondromalacia Patella and Knee Arthritis, each with its distinct characteristics and management strategies. This article aims to differentiate between these two conditions, shedding light on their pathology, age of onset, nature of pain and radiation, symptoms, investigations, and treatment options.
Chondromalacia Patella: An Overview
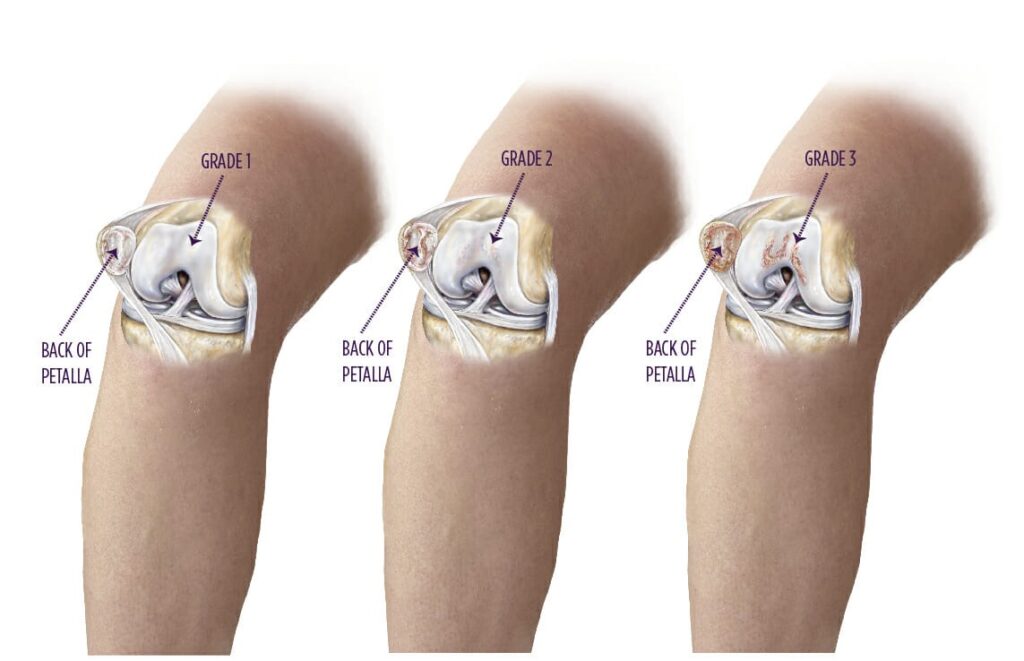
Pathology
Chondromalacia Patella, often referred to as runner’s knee, is a condition characterized by the softening and degeneration of the cartilage on the underside of the patella (kneecap). This deterioration can result from abnormal patellar tracking, overuse, or injury. As the cartilage softens, it can lead to friction between the patella and the femur, causing pain and discomfort.
Age of Onset
Chondromalacia Patella typically affects younger individuals, often occurring in adolescents and young adults. This is because it is often related to activities that place repetitive stress on the knee joint, such as running, jumping, or sports participation.
Nature of Pain and Radiation
The pain associated with Chondromalacia Patella is typically described as a dull, aching pain around or behind the patella. It is often exacerbated by activities that involve bending the knee, such as climbing stairs, squatting, or kneeling. The pain tends to be localized to the front of the knee and may not radiate to other areas of the leg.
Symptoms
Common symptoms of Chondromalacia Patella include :
- Pain when walking, running, or climbing stairs
- A sensation of grinding or grating when moving the knee
- Swelling around the patella
- Weakness in the quadriceps muscles
- Stiffness in the knee joint
Investigations
To diagnose Chondromalacia Patella, a healthcare provider may use various imaging techniques, such as magnetic resonance imaging (MRI) or arthroscopy, to visualize the condition of the cartilage and surrounding structures. Additionally, physical examinations and a detailed medical history are essential for an accurate diagnosis.
Treatment
Treatment for Chondromalacia Patella often includes :
- Physical therapy : Targeted exercises to strengthen the quadriceps muscles and improve patellar tracking.
- Activity modification : Avoiding activities that exacerbate symptoms.
- Pain management : Over-the-counter pain relievers or anti-inflammatory medications.
- Bracing : To provide support and reduce patellar stress.
- Injections : Platelet Rich Plasma and prolotherapy is an extremely effective treatment approach in early to moderate grades.Surgery is rarely necessary for Chondromalacia Patella and is typically reserved for severe cases that do not respond to conservative treatments.
Knee Arthritis: An Overview
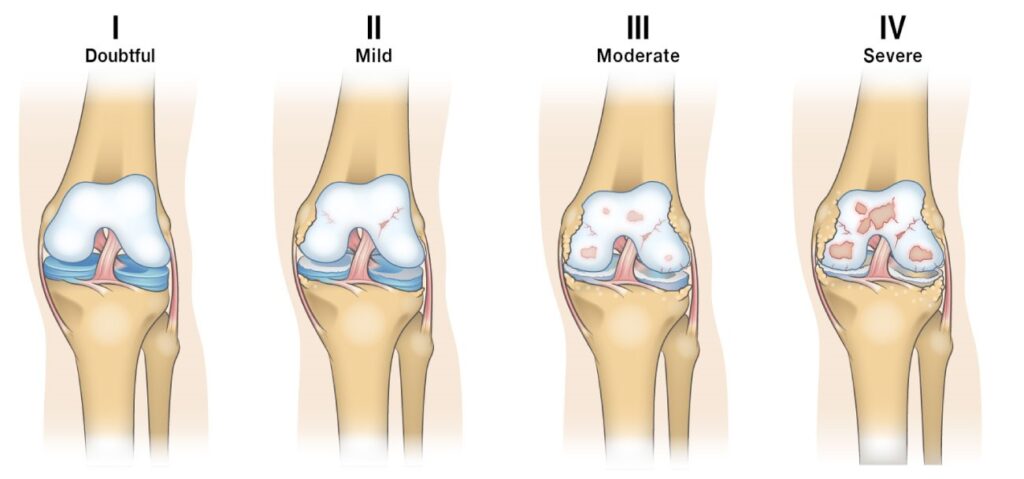
Pathology
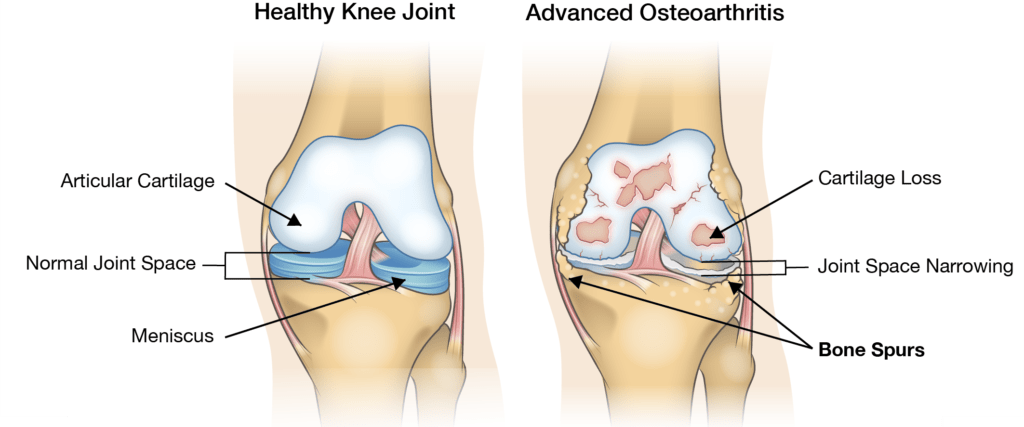
Knee Arthritis, also known as osteoarthritis of the knee, is a degenerative joint disease characterized by the breakdown of the cartilage that cushions the ends of the bones in the knee joint. This breakdown leads to pain, swelling, and decreased mobility. While it can occur as a result of aging, it can also develop following a knee injury.
Cartilage Loss/Joint Space Narrowing
Cartilage loss is one of the primary markers used in the diagnosis of osteoarthritis. People with knee osteoarthritis can experience close to double the amount of degradation compared to the level of cartilage loss in a healthy knee over the same period of time. This cartilage loss causes the space between bones in the knee joint to narrow and can lead to bone-on-bone contact in the knee, often causing severe pain and discomfort. The rate of cartilage loss varies widely among individuals so it is difficult to predict how quickly it will wear away for any one person. During everyday activities like walking, crouching, or getting up from a seated position the forces acting at the points of contact between the joints can be up to three times greater than body weight. During a squat, this number approached seven times body weight. When the bones no longer have the cushioning provided by cartilage this can cause intense pain during these activities.
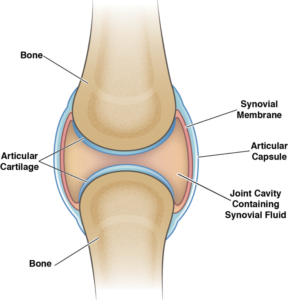
Change in Synovial Fluid
Synovial fluid is the natural lubricant that fills the joint. It allows for smooth movements, keeps the joints separated, and acts as a filter for the joint allowing the passage of nutrients while keeping out harmful substances. In cases of severe knee osteoarthritis, the synovial fluid becomes more watery and less effective as a lubricant for the joint. This causes more friction and overall wear and tear and is one of the main contributors to the cartilage loss discussed above.
Osteophyte Formation
When cartilage loss is at a point where bone-on-bone contact occurs there is often excessive bone growth in the affected compartment. These bone growths are called osteophytes (or “bone spurs”). Osteophytes can cause stiffness in the affected joint and can cause pain if they put pressure on nearby nerves. They are also often associated with misalignment of the affected knee, a common symptom of late-stage knee osteoarthritis.
Inflammation
Osteoarthritis has historically been classed as a non-inflammatory type of arthritis when compared to rheumatoid arthritis, but studies in the last decade have led to that view being reassessed as new evidence comes to light. The synovium (the area containing synovial fluid in the joint) is an area commonly affected by inflammation for people with osteoarthritis. Inflammation is usually characterized by redness, swelling, pain, and increased temperature in the area. Inflammation is caused by factors associated with osteoarthritis triggering the body’s natural immune response.
Age of Onset
Knee Arthritis is more commonly associated with older adults, typically affecting individuals over the age of 50. However, it can also develop in younger individuals, especially those who have had a significant knee injury or trauma.
Nature of Pain and Radiation
The pain of Knee Arthritis is often described as a deep, aching pain within the knee joint. Unlike Chondromalacia Patella, the pain in knee arthritis can radiate to other areas of the leg, including the thigh or calf. It is often aggravated by weight-bearing activities such as walking or standing for extended periods.
Symptoms
Common symptoms of Knee Arthritis include:
- Pain and stiffness in the knee joint, particularly after periods of inactivity
- Swelling and tenderness around the knee
- A grating or crunching sensation (crepitus) when moving the knee
- Decreased range of motion
- Weakness in the leg muscles surrounding the knee
Investigations
Diagnosis of Knee Arthritis typically involves a combination of physical examination, medical history, and imaging studies. X-rays are commonly used to assess joint degeneration and confirm the diagnosis. In some cases, MRI or CT scans may be employed to provide more detailed information about the joint’s condition.
Treatment
Treatment for Knee Arthritis is aimed at managing symptoms and improving joint function. Common approaches include:
- Medications : Pain relievers, non-steroidal anti-inflammatory drugs (NSAIDs), and disease-modifying medications may be prescribed.
- Physical therapy : To improve joint flexibility and muscle strength.
- Lifestyle modifications : Weight management, activity modification, and the use of assistive devices (e.g., canes) to reduce joint stress.
- Corticosteroid injections : To reduce inflammation and provide pain relief.
- Hyaluronic acid injections : To lubricate the joint and alleviate pain.
- Regenerative knee injections : Stem cells, Platelet Rich Plasma and Prolotherapy are often recommended for patients for early to moderate grades of knee osteoarthritis.
- Surgery : In severe cases, joint replacement surgery (total knee arthroplasty) may be considered.
Distinguishing Chondromalacia Patella from Knee Arthritis
Distinguishing between Chondromalacia Patella and Knee Arthritis is crucial for accurate diagnosis and appropriate treatment. Here are some key differentiators:
- Age of Onset : Chondromalacia Patella typically affects younger individuals, while Knee Arthritis is more common in older adults.
- Nature of Pain : Chondromalacia Patella often presents with localized, anterior knee pain aggravated by activities like squatting or climbing stairs. In contrast, Knee Arthritis typically causes deep, aching pain that can radiate to other parts of the leg and worsens with weight-bearing activities.
- Radiation of Pain : Pain in Chondromalacia Patella is usually limited to the knee, whereas Knee Arthritis pain can radiate up the thigh or down the calf.
- Symptoms : Chondromalacia Patella may be associated with a grinding or grating sensation, while Knee Arthritis often includes joint stiffness, crepitus, and decreased range of motion.
- Imaging : Imaging studies like X-rays can reveal joint degeneration characteristic of Knee Arthritis, whereas Chondromalacia Patella may require MRI or arthroscopy to visualize cartilage damage.
- Treatment : Treatment approaches differ; Chondromalacia Patella management focuses on strengthening exercises, pain relief,Prp and prolotherapy whereas Knee Arthritis treatment includes a broader range of options, including medication, lifestyle modifications, regenerative injection treatments and surgical interventions for severe cases.
Conclusion
Knee pain can significantly affect an individual’s daily life and mobility. Understanding the differences between Chondromalacia Patella and Knee Arthritis is vital for accurate diagnosis and effective treatment. While both conditions can cause knee pain, they differ in terms of pathology, age of onset, nature of pain and radiation, symptoms, investigations, and treatment options. Proper diagnosis by a healthcare specialists such as AT ALLEVIATE is essential to tailor a treatment plan that addresses the specific condition and provides the best possible outcome for the patient.





