ANATOMY AND PATHOPHYSIOLOGY

NERVE INNERVATION
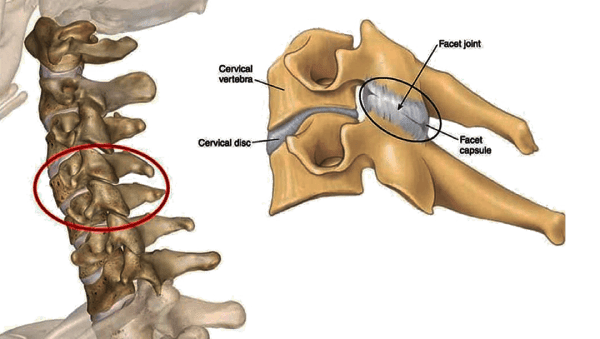
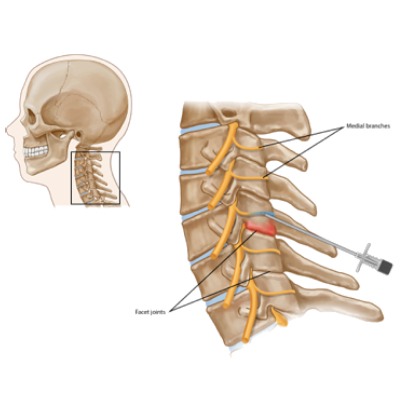
Cervical Facet Joints right from C3-C4 upto C8-T1 are supplied by medial branches of the cervical dorsal rami above and below the joint as these branches traverse around the waist of the articular pillars. Two separate branches of the C3 dorsal ramus(a medical branch called the third occipital nerve and another articular branch arising from the origin of the communicating branch or from the communicating branch itself) innervate the C2-C3 facet joint. The Atlanto-occipital and the Atlanto-axial joints( upper cervical synovial joints) are supplied by the branches of the C1 and C2 of the ventral rami. The innervation of the cervical facet joints was well described by Bogduk
ETIOLOGY
The etiology of cervical facet joint syndrome might be either traumatic or degenerative in nature.
TRAUMATIC- Traumatic causes can include fractures, dislocations and the most commonly observed “WHIPLASH INJURY” of the neck. There have been a few theories describing the mechanism behind whiplash injuries. It is believed that facet joint injury might result from two different mechanisms during impact from the rear end significant compression of the facet joints, Capsular ligament strain exceeding the physiologic limit.
It was proposed by Pearson et al[6] that the compressive forces acting across the facet joints are maximal at the time of full permissible extension of these structures. However the strain on the capsular ligaments is initiated during extension but reaches its peak as the facets move back to a neutral position from a point of maximum extension.
DEGENERATIVE
The degenerative wear and tear of osteoarthritis can also lead to painful cervical facet joints. A proposed theory explaining the etiology of Facet arthritis is based on the 3-joint complex theory. It is believed that the disc degenerate first leading to a loss of disc height. This in turn increases the stresses across the facet joints eventually bringing about arthritic changes. A study even described the setting in of facet joint arthritis 20 years after the onset of disc disease
CLINICAL FEATURES
Cervical facet joint arthritis/ Cervical osteoarthritis can exhibit a wide spectrum of symptom ranging from occasional bouts of discomfort to severe, persistent pain causing deleterious effects on the daily quality of life.
Cervical Facet Joint Pain shows the following features :

Feeling of stiffness and a dull ache rather than a sharp pain,especially in the early stages.

The onset of pain is usually gradual and slowly progresses over time

Rest helps in tiding over a flare up of pain.

Radiation of pain is often noticed to the shoulder on the same side or between the shoulder blades

Pressing down on the neck produces pain

Pain and stiffness are worse in the mornings and the individual starts feeling better as the day progresses. Aggravation in symptoms can be again seen at the end of the day

In advanced stages the pain can be so relentless that it even starts disturbing the sleep.

It is often associated with headaches especially in the back of the head
Worrisome symptoms of cervical facet joint arthritis can ensue if a nerve is impinged by osteophytes or bone spurs. This may produce symptoms of Cervical Radiculopathy like pain, tingling, numbness and even weakness in some cases. The radiation may begin at the neck and go down the shoulder, the arm and the fingers of the ipsilateral upper limb. In some cases impingement on the spinal cord due to narrowing of the central canal by bone spurs can lead to compression of the spinal cord leading to myelopathy. Myelopathy can wreck havoc with an individual’s independence and quality of life as it can lead to gait abnormalities as well as compromise in bowel and bladder function.

DIAGNOSIS
A through history must be taken from the patient. It is helpful to rule out a whiplash injury or any traumatic event leading to hyperextension of the neck. Clinical examination might be helpful in eliciting local tenderness. It is particularly helpful to carry out a complete sensory and motor testing along with the Spurling’s test to rule out signs of nerve impingement.
X rays of the cervical spine in Flexion and Extension views can give us a better picture.
Dynamic X ray imaging is used by some clinicians to see the movement and integrity of the zygapophysial joints through the range of movement.
MRI and CT scans have both found their way in the imaging, clinical decision making and Surgical planning in pathologies of the facet joints. While MRI throws light on the other soft tissue structures like the discs and the nerves, the CT captures the bony architecture well.
Diagnostic Intrarticular facet joint injections or medial branch block with local anaesthetic under fluoroscopic guidance can be further used to ascertain the facet joints as the source of pain.
AT ALLEVIATE
In addition to treating patient’s pain with anti-inflammatory injections and Radiofrequency Ablation, we generally follow up the pain relieving procedures with successive treatments of Image guided Platelet Rich Plasma with Comprehensive Prolotherapy. PrP is directed mainly at the facet joints and rest of the ligament and muscular attachments are treated with prolotherpay. We have seen phenomenal improvement in symptoms in some patients who have completed the Prp and Prolotherapy sessions and have also followed the key excercise and lifestyle modifications to aid their treatment.
Treatment for Back Pain / Back Injury
TREATMENT
Conservative treatment is initiated first to control the symptoms. These include

Adequate rest during exacerbations/flareups by limiting neck movements for a day or two till the bout of pain settles down.

Cold or ice packs are helpful during periods of active inflammation and pain. Heat can be used at other times to relax the soft tissues

NSAIDs- Anti-inflammatory medications (most commonly used are COX-2 inhibitors) are useful in relieving the pain from active inflammation

Lifestyle Modification- Incorporating exercise, stretching or some form of cardiovascular activity which does not aggravate the pain is key step in the management. Certain movement or activities that twist or move the neck in a provocative manner should be limited. Eg. Swimming is a wonderful full body workout but people with cervical osteoarthritis might have to avoid a few strokes which put undue pressure on the cervical facet joints.

Physical Therapy- The right stretching and excercise under the guidance of a physical therapist can make the neck muscles more
supple, strong and flexible preventing them from going into frequent spasms
INTERVENTIONAL PAIN MANAGEMENT

Diagnostic and Therapeutic Anti Inflammatory Injections- Cases not responding to conservative means are good candidates for Fluoroscopy guided injections. A mixture of local anaesthetic and steroid is either infiltrated into the facet joint proper or is used to administer a medical branch block for the concerned joint. If the pain comes down these injections serve as a diagnostic tool ( actually the most confirmatory tool in practice). The anti-inflammatory properties of steroids deliver the therapeutic effect which may last from a few weeks to several months. The medial branch block is chosen by many pain physicians over the direct intrarticular injection as it does not violate the joint. Some studies even indicate that the medial branch nerve blocks are seen to offer longer-lasting pain relief than facet joint injections in the cervical spine.

Radiofrequency ablation (RFA). Radiofrequency ablation or Radiofrequency Neurotomy of the nerves innervating the facet joint is a pretty popular procedure in managing facet joint pain. Candidates who have responded well to a diagnostic/therapeutic medial branch block are the ideal candidates for undergoing Radiofrequency Ablation of the Medial Branch of the dorsal rami. A minimally-invasive RFA procedure delivers heat from a needle tip to create lesions on the small nerves that feed into the facet joint.
FAQs - CERVICAL FACET JOINT SYNDROME
Cervical Facet Joint Syndrome or Cervical Osteoarthritis is similar to the arthritis-like condition that promotes back and neck pain due to joints breaking down or deteriorating. The cervical facet joint occurs only in the upper section of the spine that connects to the neck.
People suffering from cervical facet joint syndrome, a degenerative condition will experience stiffness and pain in the cervical region (neck) of the spine.
The cause of the cervical facet joint syndrome is largely caused cartilage in the joints wearing or breaking down due to old age. Injure, repetitive movements, poor posture, and other spine conditions can also develop facet joint syndrome.
A disease of cervical facet syndrome can be traumatic that causes fractures, dislocation, and it is observed as the Whiplash Injury of the neck.
Cervical facet joint arthritis/Cervical osteoarthritis signs and symptoms can vary from patient to patient. A patient can occasionally feel discomfort, pain, and be unable to perform normal activities. A patient can experience the following symptoms:
• Pain, weakness, and tingling in the areas of hand and arm
• Radiation of pain often seen on the shoulder and shoulder blades
• In advanced stages, pain can be severe with disturbed sleep
• Pain at the neck region
• Pain at the upper back affecting the shoulder
• Headaches, especially at the back of the head
• Decrease in movements or inability to move
• Pain, weakness, and tingling in the areas of hand and arm
• Radiation of pain often seen on the shoulder and shoulder blades
• In advanced stages, pain can be severe with disturbed sleep
• Pain at the neck region
• Pain at the upper back affecting the shoulder
• Headaches, especially at the back of the head
• Decrease in movements or inability to move
If you see signs and symptoms associated with cervical facet joint arthritis then you consult immediately with a doctor. A doctor will help in clinical examination that might help to determine the treatment process.
For every procedure, tests help in determining the exact treatment process. Your pain management specialist will carry out tests such as X-Ray to view the damage that causes cervical osteoarthritis. MRI and CT scans are the other imaging test to view degenerative conditions.
Conservative treatment is the best option to cure cervical facet syndrome. Most of the cases are successfully treated with non-surgical techniques.
The treatment options available are
• Resting
• Ice or cold packs
• NSAIDs
• Lifestyle modification
• Resting
• Ice or cold packs
• NSAIDs
• Lifestyle modification
Your physician recommends rest during exacerbations/flareups. It decreases inflammation by limiting neck movements for a day or two.
Applying cold or ice packs will help during active inflammation and pain. A heat pack is the other treatment option to relax the soft tissues.
With approved NSAIDs – an anti-inflammation medication, it helps relieve the pain from the active inflammation. COX-2 inhibitors are the most commonly used NSAIDs prescribed by the doctor.
It is important to incorporate an exercise program, stretching or cardiovascular activity can also help in increasing stability. With your pain management specialist and physiotherapist, you will be asked to follow an exercise routine at a limited range to avoid excessive stress
A moderate and light exercise is a part of the physical therapy program. Stretching techniques can make muscles strong and flexible.
Related Videos
Testimonials
References
[1]. Clark CR; The Cervical Spine Research Society, Editorial Committee. The cervical spine. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2005.
[2]. Pal GP, Routal RV, Saggu SK. The orientation of the articular facets of the zygapophyseal joints at the cervical and upper thoracic region. J Anat 2001;198:431-41. CERVICAL
FACET DYSFUNCTION, Mitra 773
[3]. Yoganandan N, Knowles SA, Maiman DJ, Pintar FA. Anatomic study of the morphology of human cervical facet joint. Spine 2003;28:2317-23.
[4]. Bogduk N. The clinical anatomy of the cervical dorsal rami. Spine 1982;7:319-30
[5]. Bogduk N, Yoganandan N. Biomechanics of the cervical spine part 3: minor injuries. Clin Biomech (Bristol, Avon) 2001;16:267-75
[6]. Pearson AM, Ivancic PC, Ito S, Panjabi MM. Facet joint kinematics and injury mechanisms during simulated whiplash. Spine 2004;29:390-7
[7]. Butler D, Trafimow JH, Andersson GB, McNeill TW, Huckman MS. Discs degenerate before facets. Spine 1990;15:111-3
[8]. Fujiwara A, Tamai K, Yamato M, et al. The relationship between facet joint osteoarthritis and disc degeneration of the lumbar spine: an MRI study. Eur Spine J 1999;8:396-401.
[9]. Boswell MV, Colson JD, Sehgal N, Dunbar EE, Epter R. A systematic review of therapeutic facet joint interventions in chronic spinal pain. Pain Physician. 2007;
© 2020-21 Alleviatepainclinic. All rights reserved.