PLANTAR FASCIITIS INTRODUCTION
CLINICAL ANATOMY WITH PATHOLOGICAL FEATURES
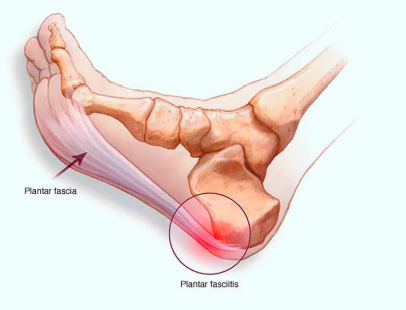
- A Fibro-fatty fat pad sits in between the heel bone and the plantar skin. The posterior tuberosity of the calcaneum gives out a medial and lateral process. The posterior tuberosity of calcaneum has a medial and a lateral processes. The medial process gives attachment to the Flexor digitorum brevis (FDB), Abductor hallucis (AH), and the medial head of Quadrates planet (QP) as well as the central band of plantar fascia.
- The plantar fascia or deep fascia of the sole, proximally has a direct fibro cartilaginous attachment to the calcaneum (an enthesis), whose central band is constant along with medial and lateral band. It has a triangular shape and develops from the medial process of the calcaneal tuberosity, and diverges distally at mid-metatarsal level into five separate strands, which are attached at the forefoot onto the plantar skin, the base of proximal phalanges (via plantar plate), the metatarsophalangeal(MTP) joints via the collateral ligaments and deep transverse metatarsal ligaments.
- Heel skin is innervated by the medial calcaneal nerve which may present with heel pain if compressed proximally (such as in tarsal tunnel syndrome). The histological features of plantar fasciitis are more suggestive of degeneration rather than inflammation. Histology in many cases is consistent with Fasciitis and Fasciosis. .information about its pathogenesis is still limited, and its histological changes are suggestive of degeneration rather than inflammation. The fascia is usually markedly thickened and gritty.
- There is evidence of spur formation in the loose connective tissue, spur trabecular forming perpendicular to the long axis and fibrocartilage orientation away from the lines of traction.
FUNCTIONS OF THE PLANTAR APONEUROSES/FASCIA
The aponeurosis is important for
- Guarding deeper structures of the foot, such as nerves and vessels.
- Maintenance of the longitudinal arch of the foot.
- Provides attachment for muscles.
- Prevents excessive dorsiflexion.
- Distributes plantar pressure during static and dynamic loading.
RISK FACTORS ASSOCIATED WITH PF
Knowledge of the risk factors of plantar fasciitis can help plan preventative and treatment strategies.
- Obesity finds it’s association with at least 60-70% of the patients suffering with plantar fasciitis. Research shows a high correlation between increased body weight and plantar fasciitis whereas the correlation of PF ( Plantar Fasciitis) with height has not shown much statistical significance.
- Calcaneal spurs are commonly associated with PF.
- Prolonged standing has been considered by some as being a contributing factor.
- Kiber et al attributed deficits in flexibility of the plantar flexor muscles leading to greater fascia stretching.
- Cheung et al propose that intense muscular contractions of the plantar flexor muscles can lead to indirect stretching of the fascia predisposing one to PF.
- Pronated foot posture and over pronation of the foot are also believed to be possible risk factors.
CLINICAL EXAMINATION
Plantar fasciitis is the most common cause of heel pain in adult population requiring medical attention. Statistics show that there is a good chance that 1 in every 10 people will experience the symptoms of plantar fasciitis at some point in their life. Historically plantar fasciitis has had quite a few synonyms namely chronic plantar heel pain, heel spur syndrome, runner’s heel, painful heel syndrome and calcaneal periostitis.

Lateral X rays of the of the ankle is a good modality for assessment of heel spur, thickness of plantar fascia, and the quality of fat pad.

Ultrasound examination in experienced hands can be very helpful when the diagnosis is unclear. In the literature, normal thickness of the plantar fascia when measured in ultrasound varies in range (mean 2–3 mm). People with chronic heel pain are likely to have a thickened plantar fascia with associated fluid collection, and that thickness values >4.0 mm are diagnostic of plantar fasciitis.

Plantar fascia thickness values have also been used to gauge the efficacy of treatments and a significant correlation has been found between decreased plantar fascia thickness and improvement in symptoms.

MRI can be helpful in resistant or doubtful cases as it can throw light on other conditions like as tarsal tunnel syndrome, soft tissue and bone tumors, osteomyelitis, subtalar arthritis, and stress fracture.

DIFFERENTIAL DIAGNOSIS
- Plantar Fascia Rupture
- Fat Pad syndrome
- Calcaneal stress fracture
- Calcaneal Bursitis/ Policeman’s heel
- Boxter’s nerve entrapment
- Medial Calcaneal Nerve Compression
- Seronegative Arthropathies
- Spinal Stenosis and L5-S1 Nerve Root Irritation
- Tumor
TREATMENT
The natural course of plantar fasciitis may last from 8-18 months making it a considerable duration of daily discomfort for the patient. Hence timely intervention can help significantly shorten the period of discomfort.
NSAIDs like naproxen or etodolac in the the acute stage are helpful in getting the pain and inflammation down.

Stretching
Calf stretching has been advocated by many experts as an important exercise in rehabilitation. Stretching may be done in the calf or plantar region. These stretches are recommended two to three times a day.

Night splints
Night splinting is done to encourage a neutral position of the ankle at night allowing passive stretching of the plantar fascia during sleep. They might be advised for 1-3 months depending on the severity.

Orthosis
Orthoses were traditionally used to reduce abnormal foot pronation. Prefabricated and customised insoles work by supporting the longitudinal arch thus helping relieving the pain.

Extra-corporeal shock wave therapy
Extra-corporeal shock wave therapy (ESWT) is believed to bring about deep tissue cavitation effect causing micro rupture of capillaries, leakage of chemical mediators, and promotion of neovascularization of the damaged tissue.[6] ESWT is carried out under intravenous sedation with or without local anaesthetic infiltration..[19,20] This modality is indicated if there is failure of other conservative measures.

Corticosteroid injection
Resistant cases are often given blind or image guided corticosteroid injections due to it’s potent anti- inflammatory effect. Ultrasound guided injections are much safer and precise [21] guiding the clinician deep into the fascia thus almost eliminating the risk of fat pad necrosis or facial rupture. Medial approach is usually preferred as it is less painful.
AT ALLEVIATE
We are primarily focussed on treating the chronic cases of plantar fasciitis we encounter with, Autologous platelet rich plasma (PRP) with Comprehensive prolotherapy. Addressing the thickened fascia with Platelet Rich Plasma, the adjoining Achilles tendon and ankle ligaments are subjected to comprehensive prolotherapy. Ideally we try to do around three sessions of this treatment at intervals of 2-3 weeks.
SURGERY
Recalcitrant cases where symptoms persist for more than 6–12 months, even after adequate conservative treatment is usually selected for Open or endoscopic plantar fascia release. Nerve conduction studies to rule out posterior tibial nerve compression should be done preoperatively.
FAQs - Plantar Fasciitis
Plantar fasciitis is a condition affecting the plantar fascia. It is an inflammation of the plantar fascia, a thick fibrous band of tissue connecting the heel to the toes.
Plantar fasciitis is the inflammation of the plantar fascia, which is a thick, fibrous band of tissue that extends from the bottom of the toes, across the heel and attaches to the inside of the foot. Other common causes of Plantar Fasciitis includes overuse, obesity, flat feet and having high arches.
The most common symptoms of Plantar Fasciitis include heel pain, pain in the heel or arch of the foot, pain that worsens during the first few steps in the morning, pain in the ball of the foot and pain in the heel after prolonged periods of standing or walking.
If you are experiencing pain in your heel, arch, or foot, you should see a doctor for Plantar Fasciitis.
Risk factors associated with plantar fasciitis include:
• Calcaneal spurs are one of the common factors associated with plantar fasciitis
• Aging - plantar fasciitis is most common in people between the ages of 40 and 60 years.
• Overweight - people with a body mass index of 30 or more are twice as likely to develop the condition.
• Excessive standing or walking
• Sedentary lifestyle
• Infrequent stretching and strengthening exercises
• Inflamed tendons in the Achilles' tendon or the plantar fascia may cause plantar fasciitis.
• prior injury and early sports participation
• Calcaneal spurs are one of the common factors associated with plantar fasciitis
• Aging - plantar fasciitis is most common in people between the ages of 40 and 60 years.
• Overweight - people with a body mass index of 30 or more are twice as likely to develop the condition.
• Excessive standing or walking
• Sedentary lifestyle
• Infrequent stretching and strengthening exercises
• Inflamed tendons in the Achilles' tendon or the plantar fascia may cause plantar fasciitis.
• prior injury and early sports participation
To detect plantar fasciitis, a doctor can check your feet for tenderness, inflammation, and pain on the bottom of your feet when you step forward. The doctor can also check for an irregularity in the way your foot hits the ground when you walk.
A clinical examination for plantar fasciitis generally includes a detailed history of the cause of pain, a physical examination, a test to determine the strength of the plantar fascia, and an X-ray.
Plantar fasciitis is diagnosed using following methods:
• History and physical exam
• X-rays
• Ultrasound examination
• MRI
• Foot biomechanics analysis
• History and physical exam
• X-rays
• Ultrasound examination
• MRI
• Foot biomechanics analysis
The most common treatment for plantar fasciitis is rest, ice and stretching the foot to relieve tightness. Other treatments may include night splint, heel cup, orthotics, and corticosteroid injections. Using anti-inflammatory medicine and physical therapy can also help.
Yes. Stretching is an effective treatment for Plantar Fasciitis. Calf stretching exercise is an effective exercise to stretch your calf muscles, but to alleviate pain and stiffness from plantar fasciitis, a mild stretch and elevation of the foot are more advisable. These stretches are advisable two to three times a day.
A night splint is an orthopedic device that is used to reduce the symptoms of plantar fasciitis. The night splint device holds your calf and ankle in a fixed position while you sleep. It is used to stretch out the Calcaneal tendon and reduce the symptoms of plantar fasciitis.
Orthosis treatments are designed to help alleviate the discomfort associated with plantar fasciitis. Orthosis prefabricated and customized insoles work by supporting the longitudinal arch to help alleviate the pain associated with plantar fasciitis.
Extra-corporeal shock wave therapy (ESWT) is a treatment for pain management and has been found to be an effective treatment for some types of foot problems, including heel spurs and plantar fasciitis. The purpose of extra-corporal shock wave therapy is to disrupt tissue without damaging it.
Yes. Extra-corporeal shock wave therapy is a non-invasive procedure that uses intense pulses of sound waves to stimulate healing on the body.
NSAIDs such as Ibuprofen, Naproxen, or Etodolac in the acute stage help get the pain and inflammation down.
A corticosteroid injection is a medication (steroid) injected into the tissue around the plantar fascia to reduce inflammation and pain. Ultrasound guided injections are guided injections in which an ultrasound is used to locate a target a specific part of the foot, heel, or ankle.
Most of the Plantar Fasciitis conditions can be treated with a conservative treatment approach. Only in a few of the cases, plantar fascia release or tibialis posterior release can be done.
Related Videos
References
[1]. Liden B, Simmons M, Landsman AS. A retrospective analysis of 22 patients treated with percutaneous radiofrequency nerve ablation for prolonged moderate to severe heel pain associated with plantar fasciitis. J Foot Ankle Surg. 2009;48:642–7. [PubMed] [Google Scholar]
[2]. Singh D, Angel J, Bentley G, Trevino SG. Fortnightly review. Plantar fasciitis. BMJ. 1997;315:172–5. [PMC free article] [PubMed] [Google Scholar]
[3]. Pfeffer G, Bacchetti P, Deland J, Lewis A, Anderson R, Davis W, et al. Comparison of custom and prefabricated orthoses in the initial treatment of proximal plantar fasciitis. Foot Ankle Int. 1999;20:214–21. [PubMed] [Google Scholar]
[4]. Cole C, Seto C, Gazewood J. Plantar fasciitis: evidence-based review of diagnosis and therapy. Am Fam Physician. 2005;72:2237–42. [PubMed] [Google Scholar]
[5]. Riddle DL, Pulisic M, Pidcoe P, Johnson RE. Risk factors for plantar fasciitis: a matched case-control study. J Bone Joint Surg Am. 2003;85-A:872–7. [PubMed] [Google Scholar]
[6]. Hossain M, Makawana N. “Not Plantar Fasciitis”: The di erential diagnosis and management of heel pain syndrome. Orthopaedics and Trauma. 2011;25(3):198–206. [Google Scholar]
[7]. Roxas M. Plantar fasciitis: Diagnosis and therapeutic considerations. Altern Med Rev. 2005;10:83–93. [PubMed] [Google Scholar]
[8]. Lemont H, Ammirati KM, Usen N. Plantar fasciitis: a degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc. 2003;93:234–7. [PubMed] [Google Scholar]
[9]. Kibler WB, Goldberg C, Chandler TJ. Functional biomechanical deficits in running athletes with plantar fasciitis. Am J Sports Med. 1991;19:66–71. [PubMed] [Google Scholar]
[10]. Cheung JT, Zhang M, An KN. E ect of Achilles tendon loading on plantar fascia tension in the standing foot. Clin Biomech (Bristol, Avon) 2006;21:194–203. [PubMed] [Google Scholar]
[11]. Cornwall MW, McPoil TG. Plantar fasciitis: etiology and treatment. J Orthop Sports Phys Ther. 1999;29:756–60. [PubMed] [Google Scholar]
[12]. Puttaswamaiah R, Chandran P. Degenerative plantar fasciitis: A review of current concepts. Foot. 2007;17:3–9. [Google Scholar]
[13]. Shazia A, Davinder P, Singh B. Plantar heel pain. Clin Focus Prim Care. 2011;5:128–33. [Google Scholar]
[14]. Alvarez-Nemegyei J, Canoso JJ. Heel pain: diagnosis and treatment, step by step. Cleve Clin J Med. 2006;73:465–71. [PubMed] [Google Scholar]
[15]. Aklirat M, Sen C, Günes T. Ultrasonographic appearance of the plantar fasciitis. Clin Imaging. 2003;27:353–7. [PubMed] [Google Scholar]
[16]. Saber N, Diab H, Nassar W, Razaak HA. Ultrasound guided local steroid injection versus extracorporeal shockwave therapy in the treatment of plantar fasciitis. Alexandria J Med. 2011;48:35–42. [Google Scholar]
[17]. Wearing SC, Smeathers JE, Sullivan PM, Yates B, Urry SR, Dubois P. Plantar fasciitis: Are pain and fascial thickness associated with arch shape and loading? Phys Ther. 2007;87:1002–8. [PubMed] [Google Scholar]
[18]. Fabrikant JM, Park TS. Plantar fasciitis (fasciosis) treatment outcome study: Plantar fascia thickness measured by ultrasound and correlated with patient self-reported improvement. Foot (Edinb) 2011;21:79–83. [PubMed] [Google Scholar]
[19]. Kudo P, Dainty K, Clarfield M, Coughlin L, Lavoie P, Lebrun C. Randomized, placebo-controlled, double-blind clinical trial evaluating the treatment of plantar fasciitis with an extracoporeal shockwave therapy (ESWT) device: a North American confirmatory study. J Orthop Res. 2006;24:115–23. [PubMed] [Google Scholar]
[20]. Mehra A, Zaman T, Jenkin AI. The use of a mobile lithotripter in the treatment of tennis elbow and plantar fasciitis. Surgeon. 2003;1:290–2. [PubMed] [Google Scholar]
[21]. Yucel I, Yazici B, Degirmenci E, Erdogmus B, Dogan S. Comparison of ultrasound-, palpation-, and scintigraphy-guided steroid injections in the treatment of plantar fasciitis. Arch Orthop Trauma Surg. 2009;129:695–701. [PubMed] [Google Scholar]
© 2020-21 Alleviatepainclinic. All rights reserved.

